By Kent R. Kroeger (Source: NuQum.com; August 1, 2021)
[All data used in this essay is available on GITHUB here.]
Last week, the Biden Justice Department decided not to open a civil rights investigation into the possibility that New York state officials intentionally manipulated data regarding nursing home deaths in an attempt to obfuscate the relatively high number of COVID-19 deaths within nursing homes.
A Justice Department letter sent by Deputy Assistant Attorney General Joe Gaeta to congressional Republican lawmakers read: “Based on that review, we have decided not to open a Civil Rights of Institutionalized Persons Act investigation of any public nursing facility within New York at this time.”
A similar letter was sent to state officials in Michigan and Pennsylvania. Apparently, the Justice Department is still considering investigations in New Jersey nursing homes.
Though New York Governor Andrew Cuomo’s office did not immediately respond to press inquiries about the Justice Department decision, it would not surprising if Governor Cuomo is feeling some vindication right now.
Unfortunately, the COVID-19 data continues to indicate something unusual may have happened in states such as New York, New Jersey, Massachusetts, Michigan and Pennsylvania where nursing homes were required to take in elderly patients previously hospitalized for COVID-19. To ensure cooperation among nursing home operators, this policy was supported by state laws or governors’ orders granting nursing homes and other long-term care facilities legal immunity from prosecutions related to COVID-19 deaths.
In the first few months of the pandemic, at least 19 states had some form of a nursing home liability waiver: Alabama, Arizona, Connecticut, Georgia, Illinois, Kentucky, Louisiana, Massachusetts, Michigan, Mississippi, Nevada, New Jersey, New York, North Carolina, Pennsylvania, Rhode Island, Vermont, Virginia, and Wisconsin.
Richard Mollot, executive director of the New York-based Long Term Care Community Coalition — a group that advocates for nursing home residents across the country — offers a grim critique of these liability waivers: “It’s basically a license for neglect.”
The state-level COVID-19 data summarized below will bear out Mollot’s concern.
It is not shocking that the Biden Justice Department wants to avoid risking political damage to Democratic governors heading into the 2022 midterm elections. But it is surprising that there is no groundswell among news organizations, government health experts, and academic researchers to demand answers on how the nursing home liability waivers may have impacted the number of COVID-19 deaths during this pandemic — if one of your loved ones was among the more than 15,800 New York nursing home residents who have died from COVID-19, you might be particularly interested in the answer.
An in-depth inquiry into the impact of these liability waiver policies does not need to imply criminal conduct. Cuomo, better than other governors, aptly defended the nursing home liability waivers when New York lawmakers began to question their rationality during the pandemic’s first wave.
At the time, Cuomo correctly noted that ICU beds in New York were rapidly being filled by COVID-19 patients and there was an urgent need to move recovering patients out of hospitals to other care environments. Wholly unfair and irresponsible are insinuations by some (including me) that Cuomo may have implemented the policy, in part, as a favor to nursing home owners who had historically been generous donors to Democratic candidates. Partisan politics brings out the worst in us all.
And if ever there is a time to avoid a partisan inquisition, an open and comprehensive investigation into the impact of the nursing home liability waivers on COVID-19 deaths would be that time. Considering four of the 19 states with nursing home liability waivers at the start of the pandemic had Republican governors, no political party can universally claim the moral high ground.
Nursing home liability waiver laws are not all the same, so assessing their collective impact is not necessarily straightforward
In an August 2020 analytic essay, I concluded that a state’s population density was the strongest correlate with the relative number of COVID-19 deaths in that state (from 18 January 2020 to 13 August 2020), but that nursing home liability waivers were also a strong correlate, associated with perhaps as many as 22,500 additional deaths over the period.
Has anything changed since then to require a different conclusion regarding these liability waivers? As with any public policy whose impact is closely monitored, bureaucrats and politicians can incorporate new learning into revising those policies. That happened with New York’s liability waiver policy soon after it became apparent — in mid-April 2020 — that a disproportionate number of COVID-19 deaths were occurring among nursing home residents. In early May, Cuomo announced that New York would no longer require nursing homes to take COVID-19 patients from hospitals.
“We’re just not going to send a person who is positive to a nursing home after a hospital visit. Period,” Cuomo said at a news conference announcing the policy change.
But the damage in human lives was already done and the extent to which other states with similar liability waiver policies changed their implementation policies appears varied. Connecticut, for example, decided to move COVID-19 positive elderly patients from hospitals to nursing homes dedicated to housing only COVID-19 patients. Healthy residents were not mixed with COVID-19 positive residents.
But, by all indications, the liability waivers remain intact, even while states have stopped moving patients from hospitals to nursing homes. In fact, some states passed their own liability waiver laws in the aftermath of New York’s tragic experience with the law. Iowa, for example, passed a liability waiver law in June 2020 giving businesses, such as nursing homes and medical facilities, protection from civil lawsuits regarding COVID-19. In July 2020, my mother — who was in her 90s — contracted COVID-19 while in an Iowa nursing home and was initially moved to a hospital, but returned to her nursing home days later, despite still suffering significant symptoms from the illness. She thankfully survived, but the experience now appears indicative of the risks associated with liability waiver laws.
Since June 2020, Iowa has had one of the highest COVID-19 death rates in the country and it is fair to ask if Mollott and other critics of liability waiver policies are correct in suggesting they are a “license for neglect.”
The circumstantial evidence suggests nursing home liability waivers cost some people their lives
It is hard to avoid the conclusion that early in this pandemic a significant number of elderly Americans died from COVID-19 because they were moved prematurely from hospital care to a nursing home.
Figure 1 (below) shows the state rankings for COVID-19 deaths per 1 million people (as of 27 July 2021). Nine out of the top 10 states in COVID-19 deaths per capita were states that had a nursing home liability waiver law in place at the start of the pandemic.
Figure 1: Top 20 U.S. states with highestCOVID-19 death rates through 27 July 2021
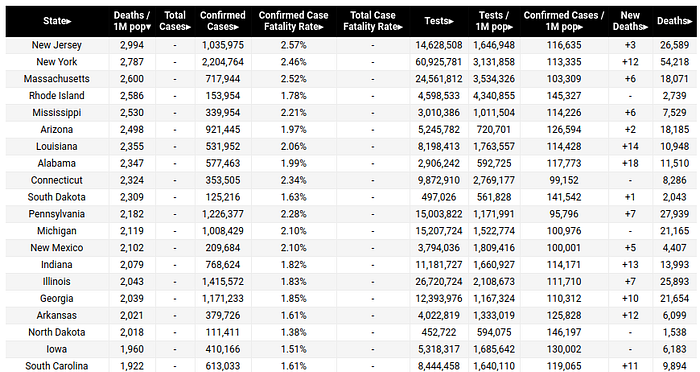
As noted, by May 2020, states such as New York, New Jersey and Connecticut had made significant changes in their implementation of nursing home liability wavier laws. In most cases, they either stopped forcing nursing homes to take on elderly COVID-19 hospital patients or segregated nursing homes by COVID-19 negative and positive residents.
Subsequently, it may be interesting to see if, statistically, there has been a noticeable drop in COVID-19 death rates in the 19 states that had liability waivers at the start of the pandemic.
Methodological Note: At least 10 states worked to pass nursing home liability waiver laws after the start of the pandemic. At the time of writing this analytic essay, I had not determined exactly how many of those states actually passed such laws and therefore leave the analysis of their possible impact on COVID-19 death rates for a follow-up essay.
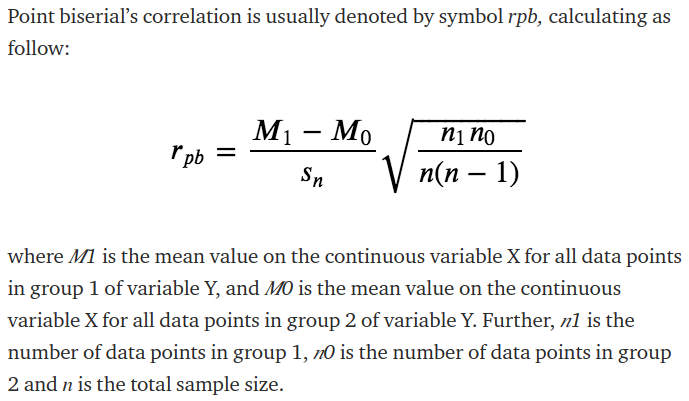
Figure 2 (below) shows the ranking of U.S. states (+D.C.) by COVID-19 death rates from 18 January 2020 to 31 May 2020 (Pandemic Phase 1). The red bars indicate states that had nursing home liability waivers laws in place at the start of the pandemic. The point biserial correlation statistic — appropriate for correlating a continuous variable with a binary variable (see Appendix A for its calculation) — between a state’s COVID-19 death rate in Phase 1 and whether it had a liability waiver law was 0.49 (significant at p<.05).
Figure 2: COVID-19 deaths per 1 million people from Jan. to May 2020 (Phase 1)
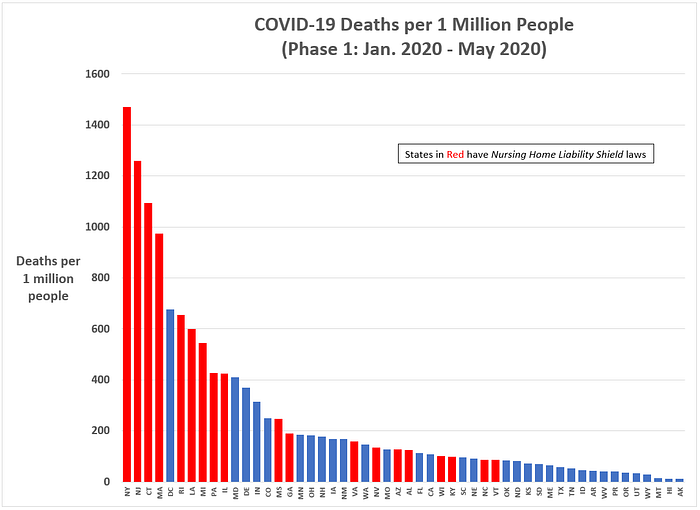
To test whether nursing home liability waiver laws continued to impact COVID-19 death rates after May 2020, I calculated the point biserial correlation using data from 1 June 2020 to 7 July 2021 (Pandemic Phase 2). The resulting statistic was 0.24 (significant at p<.10).
Figure 3: COVID-19 deaths per 1 million people from 1 June 2020 to 7 July 2021 (Phase 2)
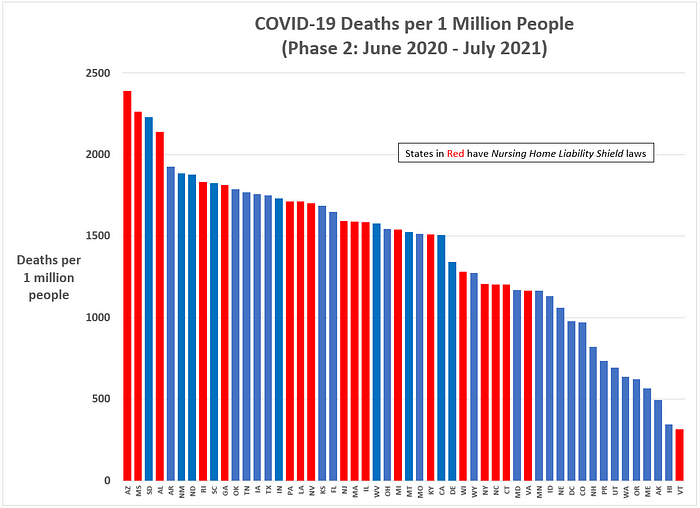
Apparently, the relationship between liability waiver laws and COVID-19 death rates weakened during the pandemic’s Phase 2, but may not have disappeared completely.
Notable in Figure 3 is how New York and Connecticut performed better than most other states in terms of COVID-19 death rates during Phase 2, but New Jersey, Massachusetts, Illinois continued to experience above average death rates. Also notable is the extremely poor COVID-19 death rate performance by states such as Arizona, Mississippi, South Dakota, Alabama and Arkansas — the explanation for which most likely goes beyond liability waiver laws and probably includes cultural, economic, and public policy factors.
Figure 4 shows a scatterplot of COVID-19 death rates by the two pandemic phases. Again, the states with liability waiver laws are in red and which tend to cluster in the upper right-hand quadrant of the scatterplot (indicating high COVID-19 death rates in both pandemic phases).
Figure 4: Scatterplot ofCOVID-19 deaths per 1 million people (Phase 1 versus Phase 2)

Nothing presented so far is conclusive about the impact of liability waiver laws, but the results are suggestive of something potentially consequential.
A mediation model of COVID-19 deaths per capita
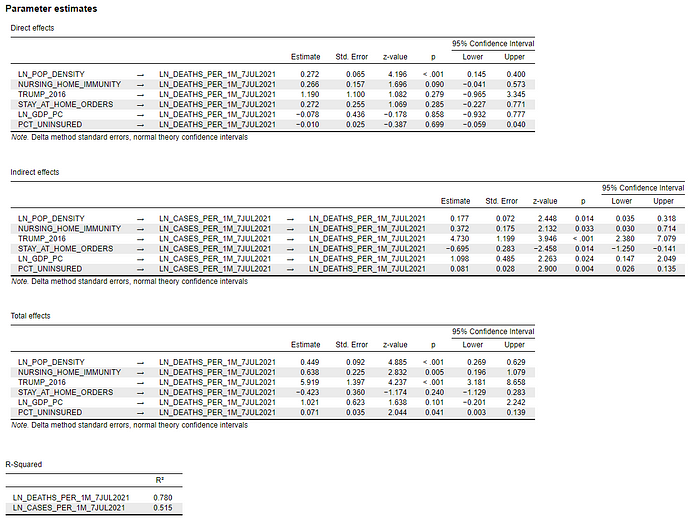
The final statistical analysis I ran attempted to account for the other major factors that may have impacted state-level COVID-19 death rates (from 18 January 2020 to 7 July 2021), including nursing home liability waivers.
The other factors considered in the model were:
- Population Density (natural log)
- Trump vote percentage in 2016 — a proxy variable for the various COVID-19 policies that tended to cluster based upon Red States vs. Blue States.
- Stay-at-Home orders — an additional policy control based on whether states ever instituted stay-at-home orders during the pandemic.
- GDP per capita (natural log) — an indication of a state’s level of economic activity
- Percent uninsured — an indication of the percentage of a state’s citizens lacking health care resources.
The model’s mediating variable through which these factors may have indirectly operated on COVID-19 death rates was the number of COVID-19 cases per 1 million people.
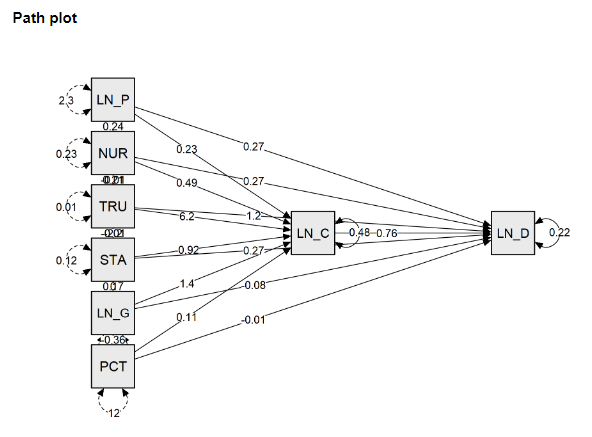
The mediation model was estimated in JASP and whose total effects results and path plot are summarized in Figures 5 and 6 below.
[The full model estimates are in Appendix B.]
Figure 5: Mediation model of COVID-19 deaths per capita — Total Effects (18 January 2020 to 7 July 2021)
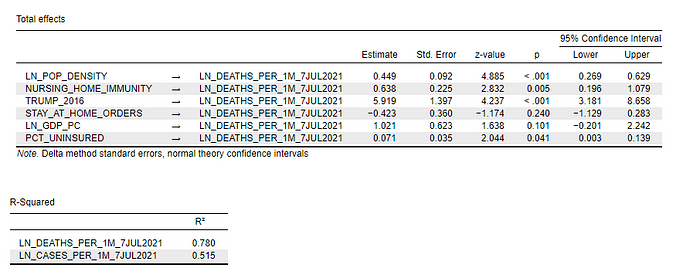
Figure 6: Pathmodel of COVID-19 deaths per capita (Jan. 2020 to 7 July 2021)
The model results indicate a strong relationship between state-level COVID-19 death rates, population density, and Red State/Blue State status (as measured by the 2016 Trump vote percentage): Densely-populated states (z = 4.89; p < .001)and Red States (z = 4.24; p < .001) had significantly higher COVID-19 death rates over the study period.
[Overall, this model explained 78 percent of the state-level variance in COVID-19 death rates.]
Densely-populated states like New York and New Jersey, however, should not feel exonerated by these results. Nursing home liability waiver states had significantly higher COVID-19 death rates. In fact, it was the most powerful correlate with COVID-19 death rates (z = 2.83; p = 0.005), after population density and Red State/Blue State status.
The other statistically significant variable in the model was the percentage of a state’s residents without health insurance (z = 2.04; p = 0.04).
While not statistically significant, there is a weak indication that economically active states — that is, state’s with high GDP-per-capita — also had slightly higher COVID-19 death rates. It is possible, an active economy inevitably brings with it higher mortality risks, irrespective of a state’s policy attempts to control the spread of a pathogen. Any benefits a state’s citizens might gain from having more financial resources to protect themselves from a dangerous virus may be dampened by the state’s higher levels of economic activity.
Final Thoughts: Our politicians, media, and government experts have a credibility and honesty problem
These results are admittedly suggestive, not conclusive. For example, methodological improvements — such as accounting for the count-data nature of the dependent variable — must be considered.
Nonetheless, it is unimaginable how anyone could look at the COVID-19 death rates and not see how major policy-related differences have been associated with variation in state-level outcomes. Equally apparent, the policy failures cut across partisan lines. Democratic-dominated states made major policy mistakes, as did Republican-dominated states.
And the previous statistical analysis doesn’t even consider the economic and social damage done by states through their COVID-19 policy strategies (lockdowns, mask mandates, crowd limits, public health care, school closings, etc.).
But the policy failures go far beyond liability waiver laws or health insurance coverage. The failures are at every level of government and society.
At one point, we had the leading virologist in the federal government tell us masks were not effective in slowing the spread of SARS-CoV-2, despite privately knowing they were, only to publicly reverse that recommendation — thereby damaging the credibility of anything he said later, no matter how factually correct. Do I harshly judge Americans now hesitant to heed Dr. Fauci’s advice about getting vaccinated? I do not.
Do I personally trust Dr. Fauci when he says the relatively new mRNA vaccine technology has no long-term health implications? For good reason, I do not— though I was still among the earliest to receive both “jabs” (Moderna) and did not hesitate to get my teenage son vaccinated (and he had previously contracted the virus).
This same government scientist slandered and shamed anyone suggesting the SARS-CoV-2 could have leaked from a Chinese lab, only to admit many months later that such a possibility could not be ruled out.
Credibility and honesty are everything in a public crisis like the COVID-19 pandemic. Occasionally being wrong is forgivable (and expected). But to fail on both accounts, as Dr. Fauci and other political-media elites have done more than once, is public service ineptitude.
Dr. Fauci should have been fired after his lies to Congress about mask-wearing — and certainly should have been fired after backtracking on the ‘lab leak’ hypothesis — but in today’s partisan environment, he’s instead lionized.
Dr. Fauci’s disingenuous behavior is more than matched, however, by the rogues gallery of Republican governors — Arizona’s Doug Ducey, Alabama’s Kay Ivey, Mississippi’s Tate Reeves, Iowa’s Kim Reynolds, and South Dakota’s Kristi Noem are the first names that come to mind — that chose to ignore common sense state measures — stay-at-home orders, mask mandates, and crowd size restrictions — at the expense of citizens’ lives.
Recall the 20 states in Figure 1 with the highest COVID-19 death rates. The high uninsured rates in southern U.S. states is bad enough — the likely product of systemic poverty and racism — but it is unfathomable how states with the population density and socioeconomic advantages of the two Dakotas and Iowa could still end up in the Top 20 for COVID-19 death rates. California Governor Gavin Newsom faces a serious recall challenge in a state that has done reasonably well, both in terms of COVID-19 deaths and economic impact, but those three Midwest governors remain overwhelmingly popular in their respective states (Iowa, South Dakota, North Dakota).
Life and politics are not always fair.
Is it coincidence the Americans who disproportionately died during this pandemic — elderly, working class, overweight, Black and Hispanic Americans — are also underrepresented by the policies coming out of our political establishment during this pandemic?
For evidence of this claim, I present nursing home liability waivers — what may be the pandemic’s worst public policy.
- K.R.K.
- I am a survey and statistical consultant with over 30 -years experience measuring and analyzing public opinion.
- Send comments to: kroeger98@yahoo.com
Appendix A: Point Biserial Correlation
Appendix B: Full Mediation Model
Dependent Variable = COVID-19 Deaths per 1 million people