By Kent R. Kroeger (Source: NuQum.com, April 9, 2020)
Key Takeaways: There is no systematic evidence that the overall quality of a country’s health care system has had an impact on the spread (morbidity rate) and lethality (mortality rate) of the coronavirus. Instead, a country’s per capita wealth and exposure to the international economy (particularly international tourism) significantly increases the spread of the virus within a country. This latter finding may be partly a function of wealthier populations being more likely to have their coronavirus-related illnesses diagnosed and treated. But it is also likely that international travel is spreading the virus worldwide.
As for the mortality rate, the story is more complicated: The single biggest driver of the mortality rate, so far, is simply the time since the country’s first coronavirus-related death. Once the virus has found a vulnerable host, the final outcome may be difficult to change (at least for now).
As for the charge by the US intelligence community that China has under-reported the coronavirus’ severity in their country, the model reported here suggests China, given its size and characteristics, should have so far experienced 10 times the coronavirus cases they have reported and a case fatality rate twice their current estimate. If they are under-reporting, as charged by the US, China may have between 33,600 to 70,000 deaths related to the coronavirus, not the 3,339 they are currently claiming.
To the contrary, it is also plausible that their aggressive suppression and mitigation efforts have successfully limited the spread and lethality of the coronavirus. The model reported here cannot determine which conclusion about China is true. Or if both conclusions have truth.
_________________________________________________________________
Its OK to feel some tentative optimism about the coronavirus pandemic. It does appear, finally, that the virus and its associated illness — COVID19 — is peaking in many of the countries hardest hit by the virus (see Figure 1).
Figure 1: New daily COVID-19 cases in Italy, South Korea, Iran and Spain
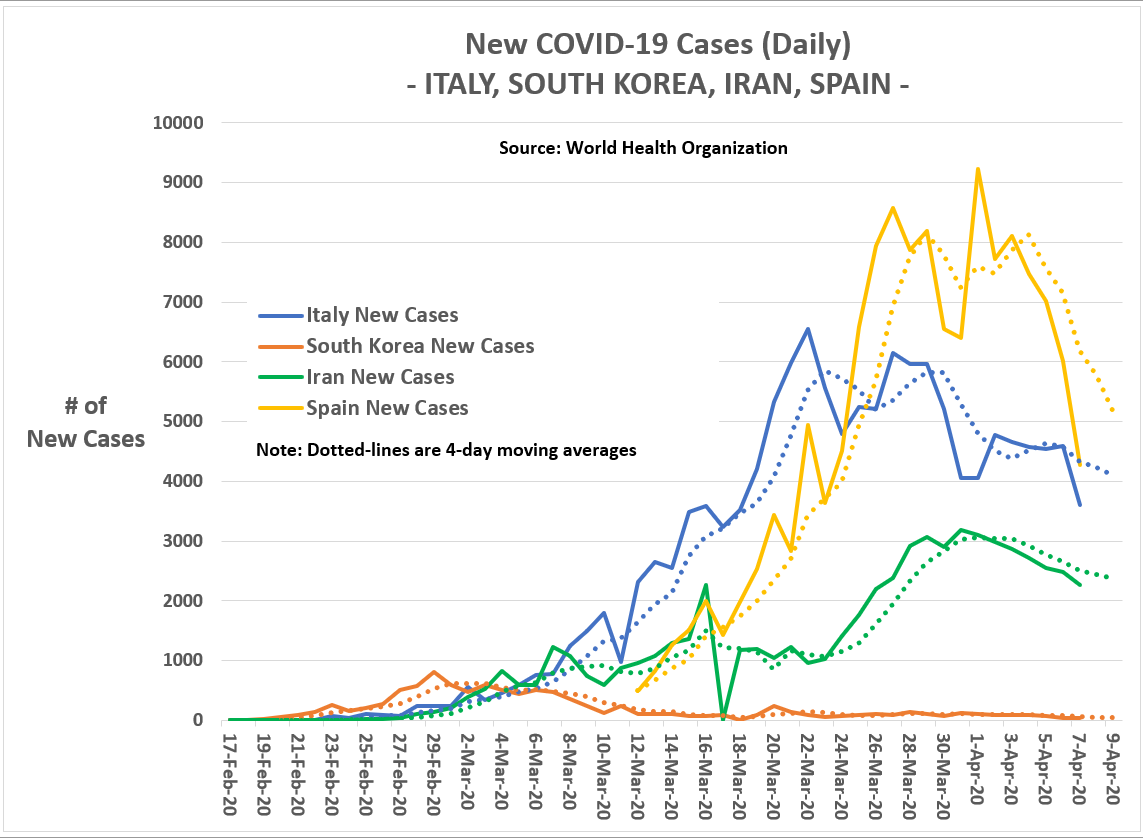
Almost a month-and-a-half after the coronavirus reached its peak in new daily cases in South Korea (around 900 cases-a-day), the virus has peaked in Italy around March 22nd, and in Spain and Iran around April 1st.
If President Donald Trump’s advisers were correct in Monday’s White House daily coronavirus update, the U.S. may also witness its peak in new daily cases within the week.
This weekend, New York, the current locus of the US outbreak, saw a significant decline in the number of new infections and deaths.
“In the days ahead, America will endure the peak of this pandemic,” Trump said Monday.
In fact, from April 6th to 7th, the aggregate US data showed its first day-to-day drop in the number of new COVID-19 cases since late March (see Figure 2).
Figure 2: Cumulative and new daily COVID-19 cases in the U.S.

In many of US states hardest hit by the coronavirus — such as New York, Washington, and California — the number of new cases each day have leveled off or declined in the past week.
These are genuine reasons for optimism. While Trump’s hope for an economic return to near-normal by Easter was overly optimistic, the possibility it could happen in early May is not.
Europe and the U.S. were caught flat-footed by the coronavirus, but it is looking increasingly like they will escape with far fewer cases and deaths than originally anticipated by many epidemiological models.
[Of course, additional waves of this virus may still occur and we may never see a true return to normal until a coronavirus vaccine is made widely available — and by widely available I mean free to everyone.]
________________________________________________________________
In this moment of cautious cheer, my questions increasingly focus on how the world measured (and mismeasured) this pandemic and what national-level factors may have suppressed and, conversely, aided the spread of the coronavirus?
Everyone has theories. Some are convinced autocratic countries (i.e., China, Iran, Venezuela, Russia) have hidden the true impact of the coronavirus on their countries. Others have declared the coronavirus proves the importance of universal health care in containing such viruses. Still others have conjectured the number of COVID19-related deaths have been over-reported by anti-Trump forces, most likely to make Trump look bad. Conversely, the national media has unofficially declared (without conclusive evidence, as usual) that the US government has been under-counting COVID19 deaths (presumably to make the Trump administration look more effective in its coronavirus response than justified).
It is speculation at this point. It will be many months — probably years — before we know what actually happened during the 2019–20 Coronavirus Pandemic. The coronavirus pandemic is still on-going, after all, and the reality is: counting the number of people with any disease or virus is genuinely hard and prone to human error.
But we can start to address some of the controversies, if only tentatively.
If we assume that the majority of countries have exercised a fairly high level of due diligence in measuring the presence of the coronavirus within their jurisdiction, we may be able to identify those countries who have been much less than honest.
Moreover, after controlling for suspected dishonest coronavirus measurement, we may also see hints at the impact of national health care systems and containment policies on the spread and lethality of the coronavirus.
________________________________________________________________
Let us start our inquiry with this premise — there are two fundamental measures of the coronavirus: (1) the number of confirmed coronavirus cases relative to the total population (morbidity rate), and (2) the number of coronavirus-related deaths as a percent of those confirmed to have the virus (mortality rate).
For simplicity’s sake, what I am calling the mortality rate is actually the case fatality rate. In reality, the coronavirus’ mortality rate is much lower than the case fatality rate as its calculation will include undiagnosed cases experiencing only minor or no symptoms.
If universal health care were ever to show its value, now is the time. The logic is simple: Countries where citizens do not need to worry about the cost of a doctor visit, the probability these citizens get tested and treated early for the coronavirus is significantly higher.
Also, countries with universal health care may also be more likely to institute broad-based coronavirus testing, thereby identifying asymptomatic super-spreaders of the virus. Subsequently, when diagnosed with the virus, these citizens will be isolated sooner from the healthy population. Furthermore, early diagnoses of the coronavirus may also improve the chances infected individuals survive the virus.
Can we see this in the data?
________________________________________________________________
Figure 3 (below) is produced directly from World Health Organization (WHO) data. The chart shows the morbidity rate of COVID-19 (i.e., frequency of COVID-19 cases per 100K people) compared to its mortality rate (i.e., deaths per confirmed case).
I’ve segmented the chart in Figure 3 into four quadrants, each defined by countries’ morbidity and mortality rates. Countries with high morbidity and mortality rates are in the upper right-hand quadrant of Figure 3 (e.g., Italy, France, Spain, Netherlands, UK and Iran.); while countries with low morbidity and mortality rates are in the lower left-hand quadrant (e.g., Russia, Japan, Pakistan, Nigeria, and India).
Figure 3: COVID-19 Cases per 100K persons versus Number of Deaths per Confirmed Case.

What does Figure 3 tell us? In truth, not much.
Ideally, a country would want to be in the lower left-hand quadrant (Low/Low) of Figure 3, right? But a simple inspection of the quadrant reveals it is occupied mainly by countries in eastern Europe, Africa, South America and southern Asia (Russia, Ukraine, Pakistan, India, Nigeria, among others) — few of which find themselves ranked by the WHO among the countries with the best health care systems. One reason for their favorable performance so far may be that the coronavirus hasn’t significantly spread to those countries yet — after all, many are in the southern hemisphere.
Here are two fair questions to ask: Are these countries performing relatively well with the coronavirus due to favorable circumstances (fewer people traveling to and from coronavirus sources like China; climatic context; stronger containment policies — an area where authoritarian governments may have an advantage; and/or better health care systems)?
Or, are some of these countries simply not deploying the resources and expertise necessary to measure the impact of the coronavirus? Do they even have the capacity to do so?
________________________________________________________________
Figure 3 begs more questions than it answers, but it still may hint at some tentative conclusions. For example, experience tells me countries clustered around the intersection of the average country-level morbidity (34 cases per 100K people) and mortality rates (3.4%) are in the accuracy ballpark. If I am feeling generous, that list includes the US and China, along with countries like South Korea, Poland and Turkey.
The countries that raise my eyebrows are the major outliers from the center cluster: Italy, Spain, UK, France, Bangladesh, Nigeria, Indonesia and India.
The variation in the coronavirus mortality rate ranges from 12 percent in Italy to near zero percent for New Zealand (a country with 1,239 confirmed cases and only one death). What could possibly explain this difference in the coronavirus mortality rate between two advanced economies? Could it be their health care systems? WHO ranks Italy’s health care system 2nd in the world, while New Zealand’s is only 41st. Russia has a reported coronavirus mortality rate of 0.8 percent and has the 130th best health care system in the world, according to the WHO.
More in line with expectations, Germany, a country given significant positive coverage for its coronavirus response — plaudits comparable to perhaps only South Korea’s — has a reported 2.1 percent mortality rate on a base of 113,296 confirmed cases.
Why such discrepancies in reported mortality rates?
Dietrich Rothenbacher, director of the Institute of Epidemiology and Medical Biometry at the University of Ulm in Germany, credits Germany’s broad-based, systematic testing as being the reason his country’s mortality figures are hard to compare to other countries.
“Currently we have a huge bias in the numbers coming from different countries — therefore the data are not directly comparable,” Dr. Rothenbacher recently told the BBC. “What we need to really have valid and comparable numbers would be a defined and systematic way to choose a representative sampling frame.”
This is where statistics — my profession — becomes critical. As Dr. Rothenbacher asserts, Germany would not have understood the extent of the coronavirus crisis without testing both symptomatic and asymptomatic cases, just as South Korea and, sadly, only a few other countries have done.
Systematic random sampling needed to be a component of every nation’s coronavirus testing program.
It wasn’t.
In New Jersey, where I live, the office of the state’s Health Commissioner told me I couldn’t get tested for the coronavirus without meeting one of the following qualifications (…it felt like a job application):
- Already being hospitalized and showing symptoms of COVID-19.
- A health care worker showing symptoms and having who been exposed to others known to have the virus
- Anyone known to be part of a cluster outbreak (one example being a recent Princeton, NJ dinner party where multiple attendees were diagnosed with the coronavirus)
- And vulnerable populations (e.g., nursing home residents).
Someone like me, a 55-year-old male with no underlying health problems but showing mild flu symptoms — low-grade fever, persistent cough, and chest congestion — cannot get tested in New Jersey.
The New Jersey testing protocol is common across the U.S. given the relative scarcity of testing kits.
________________________________________________________________
Anytime the anecdotal evidence is contradictory or unclear, I turn to data modeling — even if crude — to test some of the initial hypotheses surrounding a controversy.
The challenge with the coronavirus is the availability and data quality of the key causal factors we’d like to test in a coronavirus model for morbidity and mortality rates. In the following linear models, I tested these independent variables:
(1) GDP per capita,
(2) Health care system overall quality (according to the 2019 edition of the CEOWORLD magazine Health Care Index),
(3) Quality of health care professionals (also measured by CEOWORLD magazine),
(4) Exposure to foreign tourism (as measured by World Bank’s measure of international tourist arrivals and international tourism receipts as a percent of total exports),
(5) Exposure to East Asian trade (measured as the percent of total merchandise exports),
(6) Percentage of population over 65 years old (as measured by the World Bank),
(7) Hospital beds per 1,000 people (as measured by the World Bank),
(8) Total COVID-19 tests per 1,000 people (as measured by OurWorldInData.org), and
(9) an indicator variable for autocratic countries the U.S. government or U.S. news media have accused of under-reporting COVID-19 cases and deaths (i.e., China, Russia, Iran, Vietnam, Turkey and Venezuela).
Since countries come into the coronavirus pandemic at different points in time and are in different stages at any point in time, I also controlled for (10) the days since the first coronavirus case was confirmed, and (11) the days since the first coronavirus death occurred.
Out of necessity, I limited the data analysis to countries with reliable data on all key independent measures and with populations over 3 million people, leaving the analysis with 76 countries.
[Note: The linear models, however, were not weighted by country population size. For example, China weighted the same as Serbia in the following models.]
The estimated linear models for morbidity and mortality rates are reported in the Appendix below.
Figures 4 and 5 show the model predictions for each country versus the actual morbidity and mortality rates. In the morbidity model graphic (Figure 4), I only show a selection of key countries in order to simplify the data presentation.
Figure 4: Predicted versus Actual COVID-19 Cases per 100K Persons for Selected Countries (as of 4 APR 2020).
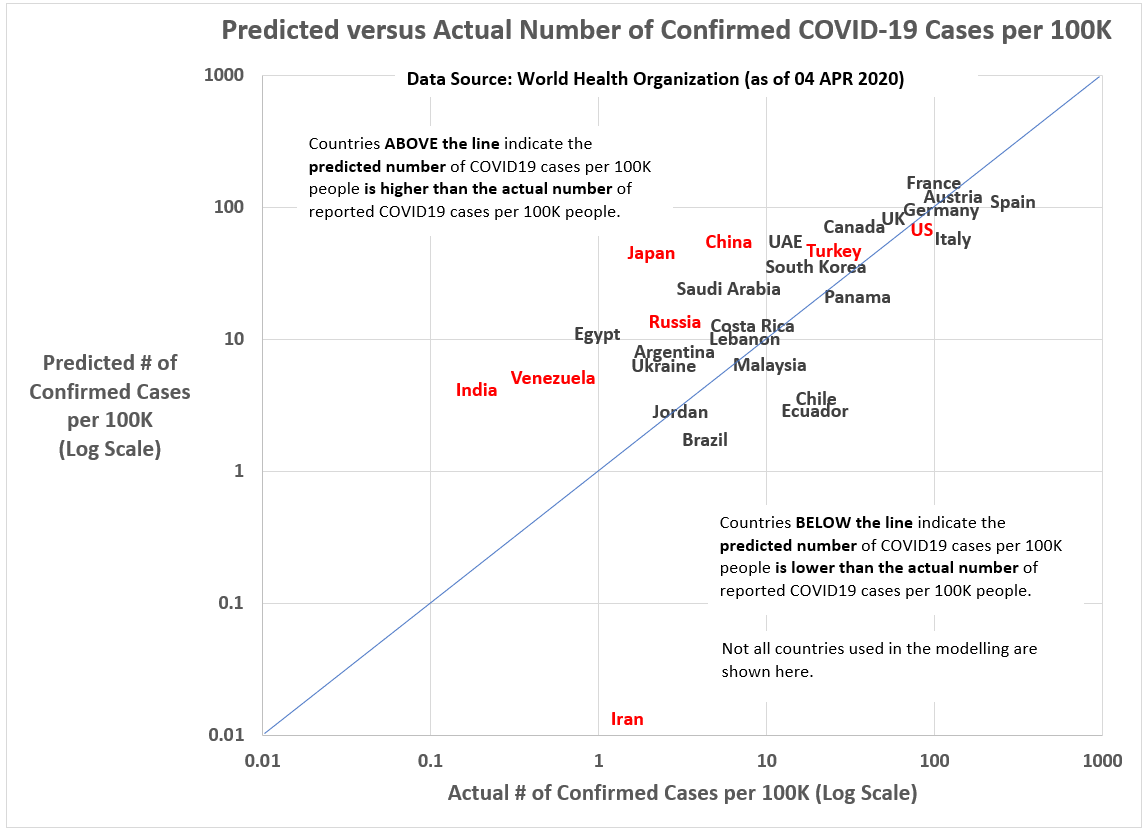
Figure 5: Predicted versus Actual COVID-19 Deaths per Confirmed Cases (as of 4 APR 2020).
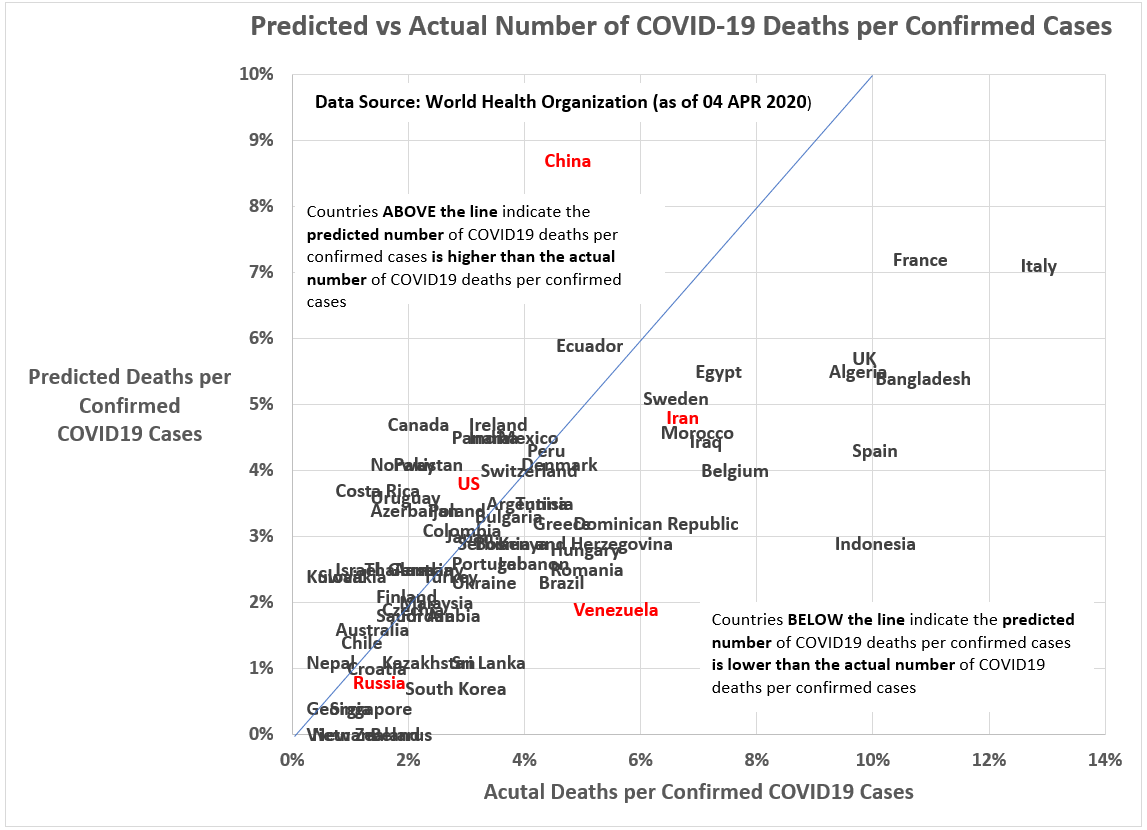
On the issue of autocratic countries (who are also U.S. adversaries), there is circumstantial evidence that Venezuela, China and Russia have fewer COVID-19 cases than we would expect given their key characteristics, even while their deviance as a group is not statistically significant.
For example, China may have 10 times the coronavirus cases they have officially reported and a mortality rate twice their current estimate. If true, China may have between 33,600 to 70,000 deaths related to the coronavirus, not the 3,339 they are currently claiming.
Likewise, Russia may have 19,500 coronavirus cases, not the 10,031 they have reported to the WHO and Venezuela may have 1,625 cases, not 167 cases.
Even if, according to the model, the reported numbers for China, Venezuela and Russia are low, we can’t rule out the possibility they are low because these countries have done a superior job containing the virus.
Perhaps the most puzzling (and saddest) case is Iran. Our model suggests Iran has experienced far more COVID-19 cases than we would expect given its characteristics. The most recent WHO numbers for Iran are 66,220 confirmed cases and 4,110 deaths.
Has Iran done an especially poor job of containing the virus or are they measuring more comprehensively than other countries? Unfortunately, my model can’t settle that point.
Final thoughts
I anticipated when I started looking at the coronavirus in 76 countries that the quality of their health care system s— starting with affordable, universal health care — would show up as a significant factor in distinguishing between countries that successfully took on the coronavirus pandemic (e.g., South Korea, Germany, Singapore, and Japan) and those less successful (e.g., Italy, Spain, France, UK and Iran).
While the number of hospital beds per 1,000 people does correlate significantly with lower mortality rates (see Appendix, Figure A.2), the overall quality of a country’s health care system did not. In fact, countries with the best compensated medical professionals actually have higher coronavirus mortality rates.
The coronavirus has hit Europe (and China) the hardest. In Italy, the high percentage of elderly helps explain its high volume of cases, but that can’t be the only explanation. And isn’t just that advanced economies have put more effort into measuring the occurrence of the virus in their communities that explains this fact. The coronavirus has found disproportionately more friendly hosts in these societies. We may have to accept that the coronavirus is one of the evolving risks associated with high disposable incomes and deeps global connections through trade and tourism.
I know this: I will never go on a cruise ship ever again.
Theories on why some countries handled the pandemic better than others are also plentiful. The most compelling analysis may have occurred while the pandemic was just starting.
Writing in early March, Chandran Nair, founder and CEO of the Global Institute for Tomorrow, may have come up with the best explanation still. “Strict and centralized enforcement of lockdowns, quarantines, and closures are the most effective way to contain the virus,” wrote Nair. “What’s emerged from the coronavirus crisis is the fact that some states are equipped to handle this type of action, and some are not — and it has little to do with development status.”
Or, more cynically, could we conclude that one of the costs of emphasizing individual freedom is that when collective action is necessary — including a strong, central state response — Europeans and Americans answer the call by hoarding toilet paper and Jim Beam?
I’m not quite there yet. For one, I don’t believe Nair fully appreciates how the modern state and elites consolidate their power during these uncertain times, and how this can leave even more people vulnerable economically and physically to the next pandemic — and there will be another one. Second, for every example of state power getting this done quickly and efficiently, there are dozens more where greed, incompetence, and arrogance lead the state to do more damage than good. Before we give the modern state more power, let us think this through some more first.
Here is what our governments and scientific community should be doing…
If this global pandemic ends relatively soon — as it appears it might — our governments and health researchers must immediately resolve themselves to understand how many people really did get infected by the coronavirus and how many actually died from its consequences.
Currently, we have a global mish-mash of epidemiological data of unknown quality or generalizability. Only probability-based sample studies can give us the real numbers and it is only with those numbers that we can really sit down and decide: What worked and what was a total waste of time and resources?
- K.R.K.
Data used in this article are available by request to: kroeger98@yahoo.com
APPENDIX: The Linear Models
Figure A.1: Linear Model for Confirmed COVID-19 Case per 100K Persons (Morbidity)
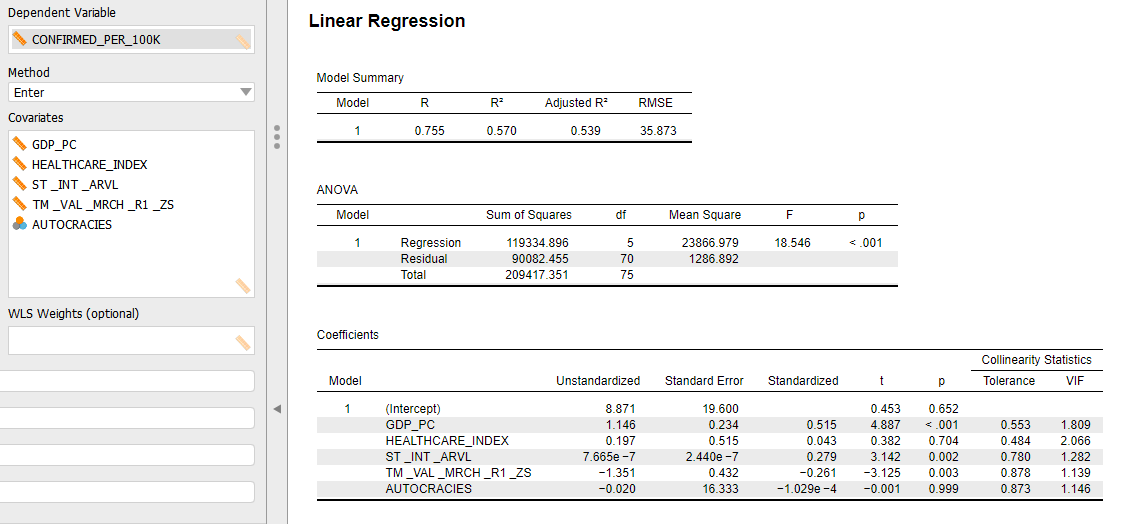
Figure A.2: Linear Model for COVID-19 Deaths per Confirmed Cases (Mortality)

