By Kent R. Kroeger (Source: NuQum.com; February 14, 2022)
Recently, Dr. Anthony Fauci declared the COVID-19 pandemic in the U.S. is “exiting the full-blown stage.”
Unfortunately, Dr. Fauci, like the rest of the medical and scientific community, has been more hostage to the coronavirus than a prescient sage as to its future trajectory.
Like a broken analog clock, Dr. Fauci may be right this time, but what a price the world continues to pay for a virus whose behavior often has been unpredictable and whose origins still remain unknown.
However, getting more attention than Dr. Fauci’s declaration about the next phase for COVID-19 was a working paper (i.e., not peer-reviewed) by three economists who conducted a meta-analysis on the effects of public policy on COVID-19 mortality. In this study, economists from Johns Hopkins University, Lund University (Sweden), and the Center for Political Studies in Copenhagen, Denmark — Jonas Herby, Lars Jonung, and Steve H. Hanke — found that “lockdowns in Europe and the United States only reduced COVID-19 mortality by 0.2 percent on average.”
Apart from the predictable efforts by news media elites to smear the credentials of the study’s authors and the intellectual value of a non-peer-reviewed working paper, sober academics and medical experts found the study interesting but far from conclusive. [For example, the study only covered outcomes during 2020.]
Dr. Vinay Prasad, MD MPH, offers a balanced perspective on the this new lockdown study: “(This) early meta-analysis suggests (lockdowns) didn’t do that much. I don’t find it that incredible but I also think it’s not the right moment to do a meta-analysis because the lockdown’s effect is a massive perturbation on the economy and society (and) it’s not just about the short-run mortality. What about the long-run mortality? What about the mortality you’re paying for down the road because of all the disruptions to society?”
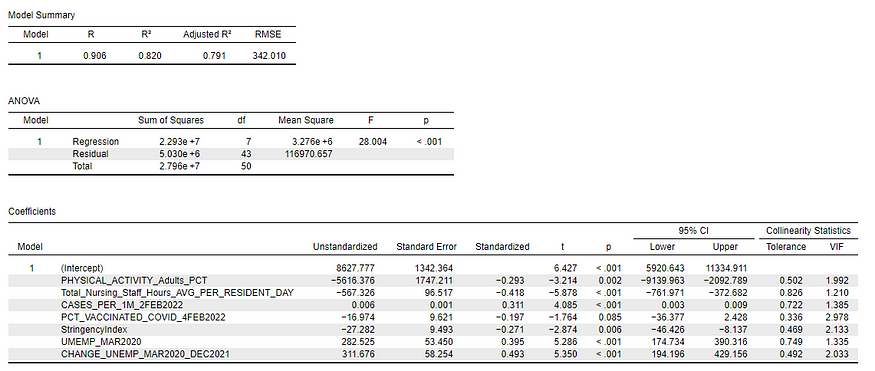
A common analytic tool employed in the studies analyzed by Herby, Jonung, and Hanke was Oxford University’s Covid-19 Government Response Tracker (OxCGRT) which collects systematic information on policy measures that governments have taken to tackle COVID-19. Included in their tracking data is a “stringency index” summarizing these policy measures for each U.S. state which is computed on a daily basis and made available to the public on GITHUB.
According to the creators of the OxCGRT Stringency Index, the index summarizes the strictness of COVID-19 policies that primarily restrict people’s behavior, including containment, closure, economic, health system and vaccination policies.
[All variables used in this analysis are available in my personal GITHUB repository or can be obtained directly from the original sources listed at the bottom of Figure 2.]
Figure 1 shows 12 selected U.S. states to represent three levels of the stringency index (High Stringency States, Medium Stringency States, and Low Stringency States).
Figure 1: Stringency Index scores for selected U.S. states from February 1, 2020 to February 2, 2022
On its face, the OxCGRT Stringency Index appears to strongly correlate with a common understanding of the states that have implemented restrictive COVID-19 policies and those that did not during this two-year pandemic.
A linear model of state-level COVID-19 death rates
Is there any evidence that stringent state-level COVID-19 policies helped reduce death rates?
Since it is unwise to make causal statements in the context of a linear model using aggregated, cross-sectional data, the answer is an emphatic ‘maybe.’ But the associations in the state-level COVID-19 data are strong enough to increase the plausibility of such conclusions.
[In general, I tried to avoid causal statements in this essay and preferred to use terms such as ‘association’ and ‘correlation.’]
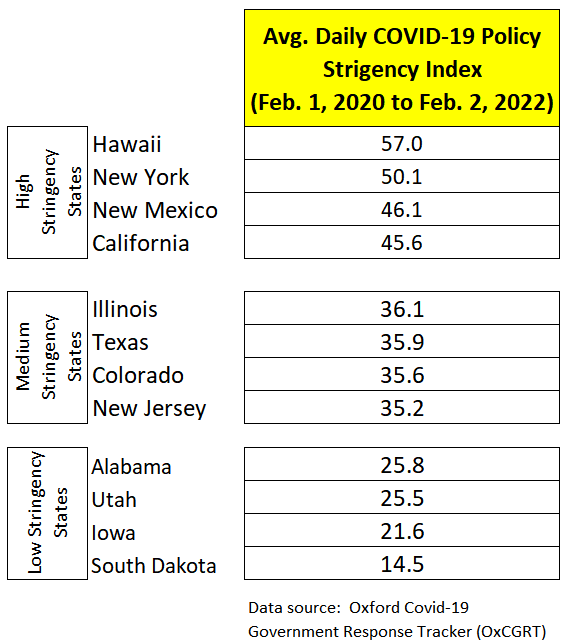
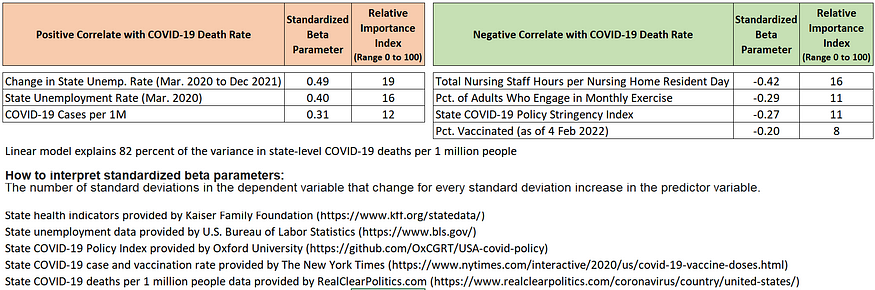
Using the variables displayed in Figure 2, I estimated a linear model to explain state-level variations (51 cases) in the number of COVID-19 deaths per 1 million people.
[Model estimates and diagnostic measures can be seen in the Appendix below. More detailed diagnostics are available upon request.]
Figure 2: The relative importance of predictor variables on state-level COVID-19 death rates from February 1, 2020 to February 2, 2022
According to the linear model, state-level unemployment rates at the beginning of the pandemic, changes in those unemployment rates between March 2020 and December 2022, and the number of confirmed COVID-19 cases (per 1 million people) are positively associated with higher state-level death rates. In other words, states with relatively weak economies heading into the pandemic and states that experienced the most economic stress during the pandemic have significantly higher death rates. In fact, they are the two variables most associated with COVID-19 death rates.
But what factors helped to lower state-level COVID-19 death rates?
Among those factors which associate with lower state-level death rates, the number of nursing staff hours per nursing home resident day appears to be the strongest, followed by aggregate measures of people’s exercise habits, the strictness of COVID-19 policies, and a state’s vaccination rate.
By interpreting the standardized regression coefficients in Figure 2, the concrete impact of the predictor variables are stunning.
For example, given that state-level COVID-19 death rates have a standard deviation of 740 deaths per 1 million people, a one standard deviation increase in the unemployment rate change associates with an increase of 363 deaths per 1 million people (or about 117,600 nationally if the unemployment rate change is applied to all 50 states and the District of Columbia).
If every state entered the pandemic with a higher unemployment rate by one standard deviation, the COVID-19 death rate might have been higher by 296 deaths per 1 million (or about 96,000 people).
By comparison, a one standard deviation increase in the stringency index associates with 200 fewer deaths per 1 million people (or about 65,000 people nationwide).
Cautionary note: Due to the high level of collinearity between state-level vaccination rates and COVID-19 stringency policies, it is preferable not to interpret their standardized coefficients separately and more instructive to combine these parameters to estimate their combined impact.
When we do that, it appears the reduction in COVID-19 deaths rates associated with higher vaccination rates and stronger COVID-19 policies is comparable in their impact to similar changes in unemployment rates.
The implication is that policymakers in the future would be smart to explicitly weigh the potential costs and benefits of those COVID-19 policies before making decisions. Through their impact on state economies, strict COVID-19 measures (such as lockdowns) have the potential to kill as many people as they save.
Final thoughts
A complete analysis of the impact of policy choices on COVID-19 death rates should also consider “collateral” deaths, which are deaths not directly related to COVID-19 but the result of strains on hospital resources such as ICU bed utilization rates and staffing availability.
This analytic augmentation would bring to the forefront the question of the total impact of the unvaccinated on state-level death rates.
In other words, the unvaccinated not only increase their personal risk of dying from COVID-19, but they increase the probabilities that other people will die of other causes when hospital and ICU beds are filled to capacity.
How many collateral deaths should be added to the current U.S. COVID-19 death count of almost 950,000 people?
A credible estimate of collateral deaths comes by way of a statistical model computed at the Centers for Disease Control and Prevention (CDC) which calculates the number of “excess” deaths occurring in the U.S. each week. Through these models, the CDC estimates “excess” deaths caused by COVID-19 and “excess” deaths by other causes.
Since the widespread availability of the COVID-19 vaccines after March 2021, the CDC estimates almost 80,000 non-COVID-19 “excess” deaths have occurred through January 1, 2022, almost all of which occurred during COVID-19 surge periods when the most stress was placed on hospital resources (beds, staff availability, etc.). Even if we deduct the probable impact of vaccinated people hospitalized for COVID-19 during this period, the unvaccinated still account for about 66,000 collateral deaths, according to the CDC numbers.
That is a big number which accounts for around three percent of all U.S. deaths during that period, or about 270 collateral deaths per day.
When President Biden said last July that anti-COVID-19 vaccine propagandists are “killing people,” he was articulating what most fully vaccinated Americans believe — the unvaccinated are indirectly guilty of killing thousands of their fellow citizens.
Was he right in saying that?
In a simplistic sense, yes, but not if one rightfully considers why so many Americans remain skeptical of the COVID-19 vaccines, effective as they are in preventing severe illness from the virus.
As I’ve written elsewhere, despite my own aggressive eagerness to vaccinate myself and my family, I understand why many people are resistant to receiving these vaccines.
The reasons are easy to list:
(1) The COVID-19 mRNA vaccines are based on a new technology with debatable levels of long-term research to add confidence in their widespread use,
(1) The mainstream U.S. news media too often serves partisan interests and subsequently is untrustworthy to dispense non-partisan public health recommendations according to millions of Americans.
(2) The U.S. government’s acquiesced to pharmaceutical companies’ insistence on liability immunity for the COVID-19 vaccines which were developed under President Trump’s taxpayer-financed Operation Warp Speed.
(3) The pharmaceutical industry’s ongoing intransigence in releasing their full vaccine testing data to independent researchers.
(4) Research suggesting the risks associated with the COVID-19 vaccines and myocarditis incidence among young males (i.e., they have a minimal risk of dying from COVID-19 and are more likely to experience myocarditis [heart inflammation] from the receiving the vaccines than from the catching the virus itself).
(5) Two scientists from the Food and Drug Administration’s vaccine advisory committee resigned last year over what they believed to be a rushed (‘political’) decision to recommend booster shots in relatively young populations. Writing with a group of other scientists in a September 2021 Lancet editorial, they said: “Although the benefits of primary COVID-19 vaccination clearly outweigh the risks, there could be risks if boosters are widely introduced too soon, or too frequently, especially with vaccines that can have immune-mediated side-effects (such as myocarditis, which is more common after the second dose of some mRNA vaccines [footnote],or Guillain-Barre syndrome, which has been associated with adenovirus-vectored COVID-19 vaccines [footnote]). If unnecessary boosting causes significant adverse reactions, there could be implications for vaccine acceptance that go beyond COVID-19 vaccines. Thus, widespread boosting should be undertaken only if there is clear evidence that it is appropriate.
According to Dr. Prasad, as yet, there is no persuasive evidence suggesting that boosting is necessary in healthy people between the ages of 12 and 50.
I don’t expect unvaccinated Americans are closely following the scientific debates over COVID-19 vaccines in medical journals, but I am constantly amazed in my interviews with the unvaccinated how often they possess at least a basic familiarity with some of the more complicated issues within the vaccine research community (e.g., myocarditis).
Yes, misinformation is abound about COVID-19 in the cyberverse — but so is a lot of valid information finding its way into the everyday conversations people have over these vaccines and the COVID-19 pandemic in general.
Some people want to assume the unvaccinated are stupid. I believe the exact opposite is true — they are awash in information and given their overactive levels of distrust and skepticism, are over-thinking what should be a fairly simple decision.
Furthermore, I find it immoral to incriminate the unvaccinated when other European countries with a similar percentage of unvaccinated still have a substantially lower number of COVID-19 deaths per capita.
According to the New York Times, 65 percent of Americans are fully vaccinated, which is comparable to Europe (64%) as a whole.
And, yet, when we observe countries with similar vaccination rates to the U.S., they have substantively lower COVID-19 death rates:
Netherlands — 71% vaccination rate (1,242 deaths per 1M)
Greece — 69% vaccination rate (2,300 deaths per 1M)
Switzerland — 68% vaccination rate (1,532 deaths per 1M)
Austria — 68% vaccination rate (1,624 deaths per 1M)
Israel — 66% vaccination rate (1,066 deaths per 1M)
U.S. — 65% vaccination rate (2,882 deaths per 1M)
Why are they doing better?
It is still too early to draw strong conclusions when the pandemic is ongoing. But early research is finding that a health care system’s characteristics have helped some countries better handle the exigencies of the COVID-19 crisis.
Among those characteristics are country’s health profile, the number of nurses and doctors, the availability of hospital and ICU beds, and the level of trust citizens hold towards their fellow citizens, government, and health care experts.
The U.S. health care system is left wanting on these factors.
As evidence, since 1960, the U.S. has seen a consistent decline in the number of hospital beds per 1,000 people. According to World Bank data, the U.S. went from 7.9 hospital beds in 1970 to 2.9 in 2017.
The U.S. clearly wasn’t preparing for a future pandemic when it allowed so many rural hospitals to close over the past 50 years.
When comparing the European countries with similar COVID-19 vaccination rates to the U.S. by the number of hospital beds per one thousand people, the U.S. comes in dead last, according to the World Bank:
Netherlands — 3.2 hospital beds per 1K
Greece — 4.2 hospital beds per 1K
Switzerland — 4.6 hospital beds per 1K
Austria — 7.3 hospital beds per 1K
Israel — 3.0 hospital beds per 1K
U.S. — 2.9 hospital beds per 1K
But it is not just hospital beds that put the U.S. at a disadvantage in handling the coronavirus pandemic, it is a health care system in which job loss and financial insecurities drive too many citizens to forgo early and sometimes life-saving medical care.
The U.S. was not pandemic-ready in early 2020, and that is not the fault of the unvaccinated — it is the fault of our political, news media, health insurance, and medical community leadership.
Before shaming and blaming the unvaccinated — which doesn’t vaccinate one person and most likely leads to greater resistance to the jab — would it not make more sense to address the structural problems in a health care system where the most economically vulnerable suffer disproportionately during a national health crisis?
If anything, we all share in the blame for a national health care system that has been outperformed by Mexico in the COVID-19 pandemic (2,823 deaths per 1M vs 2,386 deaths per 1M, respectively). If we were doing as well as Mexico — where about 60 percent of its citizens are fully vaccinated — the U.S. would have 144,000 fewer deaths right now.
But it is so much easier just to blame the unvaccinated.
- K.R.K.
Send comments and data requests to kroeger98@yahoo.com
Appendix: Linear model estimates and selected diagnostics.