By Kent R. Kroeger (Source: NuQum.com; July 6, 2022)
Cross-national data analyzed in this essay can be found on Github==>Here
“Pandemic or not, America has the best healthcare in the world,” declared a 2020 cross-national study of COVID-19 survival rates by the Acton Institute, a free-market-promoting think tank. “When President Donald Trump fell ill with COVID-19, there was absolutely no contemplation of moving America’s head of state to another country to receive healthcare services.”
Unintentionally, the Acton Institute’s study highlights exactly why the U.S. healthcare system is not the world’s best by most objective measures. The healthcare received by our president is not the same healthcare received by a large percentage of Americans.
And no issue has been a bigger motivator for this blog than the systemic underperformance of the U.S. healthcare system.
Although my family has adequate insurance coverage, unpredictable healthcare costs could compromise our financial well-being in a jiffy moment.
The COVID-19 pandemic brought that possibility to the fore when my entire family came down with the novel coronavirus within days of one another, and while none of us suffered too greatly from its effects, the night I had a 103-degree fever and prayed for a quick and merciful death suggests it could have turned out differently had I not been vaccinated and in reasonably good health.
Still, it would have taken just one extended hospital stay among us to have fundamentally changed our financial well-being.
On average, a one-night hospital stay in the U.S. costs $11,700. For most Americans, health insurance covers most of that cost, but what about for the 31 million uninsured or 75 million underinsured? The answer is often tragic.
According to Debt.org, between 60 and 65 percent of all bankruptcies are due to medical expenses, and a 2018 study by The Commonwealth Fund found that 41 percent of underinsured adults had postponed important health care due to cost. Even among adequately insured Americans, 23 percent reported delaying needed care.
Early within the COIVD-19 pandemic, the U.S. Centers for Disease Control and Prevention (CDC) warned that delaying care could increase the country’s morbidity and mortality rates associated with COVID-19. In a survey conducted by the CDC in June 2020 discovered that “an estimated 40.9 percent of U.S. adults have avoided medical care during the pandemic because of concerns about COVID-19, including 12.0 percent who avoided urgent or emergency care and 31.5 percent who avoided routine care.”
A policy analysis by Yale’s Center for Infectious Disease Modeling and Analysis appears to confirm the CDC’s concern about delayed care. “Universal healthcare could have alleviated the mortality caused by a confluence of negative COVID-related factors,” concluded the June 2022 study published in Proceedings of the National Academy of Sciences USA. “Incorporating the demography of the uninsured with age-specific COVID-19 and nonpandemic mortality, we estimated that a single-payer universal healthcare system would have saved 212,000 lives in 2020 alone. We also calculated that US$105.6 billion of medical expenses associated with COVID-19 hospitalization could have been averted by a Medicare-for-All system.”
The same study concluded 330,000 American lives could have been saved over from 2020 to 2021 had this country had a universal healthcare system.
But as I would tell students, rarely can one study end the discussion on an important policy-related question, and has solid as the policy analysis methodology was for the Yale study, a cross-national comparison of COVID-19 death rates is warranted.
A Comparison of National Healthcare Systems (Type vs. Quality)
Perhaps it is analytic hubris to believe it is possible to categorize national healthcare systems into a small number of mutually-exclusive categories, but contributors to Wikipedia gives it a decent shot:
- Universal government-funded health system (e.g., Australia, Brazil, Canada, Denmark, Norway, Sweden, Taiwan, and U.K.)
- Universal public insurance system (e.g., Belgium, China, France, India, Japan, Russia, and South Korea)
- Universal public-private insurance system (e.g., Austria, Germany, Mexico and Turkey)
- Universal private health insurance system (e.g., Israel, Netherlands, and Switzerland)
- Non-universal insurance system (e.g., Indonesia, Nigeria, Pakistan, Uganda, and U.S.)
However, on its face, this categorization appears problematic for analytic purposes as it is hard to agree that Pakistan and the U.S. have similar healthcare systems, despite both being categorized has having non-universal insurance systems, or that South Korea and China have objectively similar universal public insurance systems.
Consequently, during the model-building process to explain cross-national differences in COVID-19 death rates, the type of healthcare system did not achieve consistent statistical significance after controlling for other national factors such a population size, age distribution, vaccination rates, and GDP per capita. [See the full linear model estimates for the model including controls for healthcare system types in Appendix A.]
In contrast, the quality of a nation’s healthcare system, as measured in a 2021 global survey of 196,000 respondents conducted by the Global Business Policy Institute (GBPI) in partnership with CEOWORLD magazine, proved consistently significant in explaining variation in COVID-19 death rates.
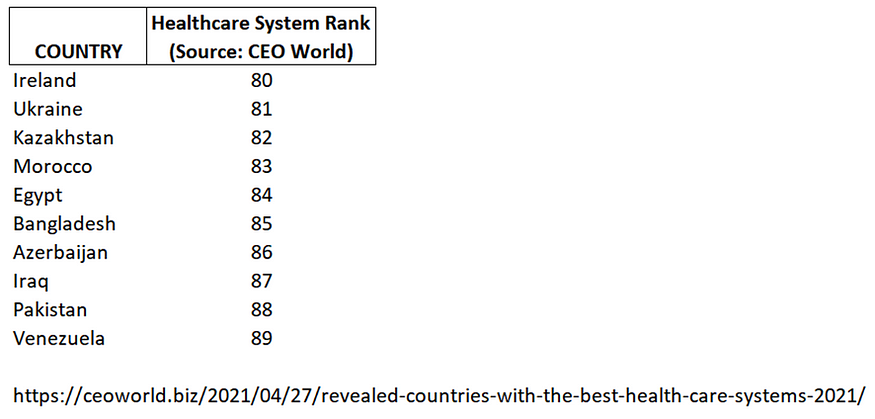
Figures 1a-b display the Top and Bottom 10 healthcare systems in 2021, according to GBPI and CEOWorld Magazine. Topping the list are South Korea, Taiwan, Denmark, Austria and Japan. Of the Top 10 healthcare systems, three of five system types were represented (Universal government-funded health system, Universal public insurance system, Universal public-private insurance system). Conversely, two of the Bottom 10 countries had universal government-funded healthcare (Ireland and Ukraine), while the remaining countries in the Bottom 10 had non-universal healthcare or could not be classified.
Figure 1a: Top 10 healthcare systems in the world (Source: CEOWorld Magazine)
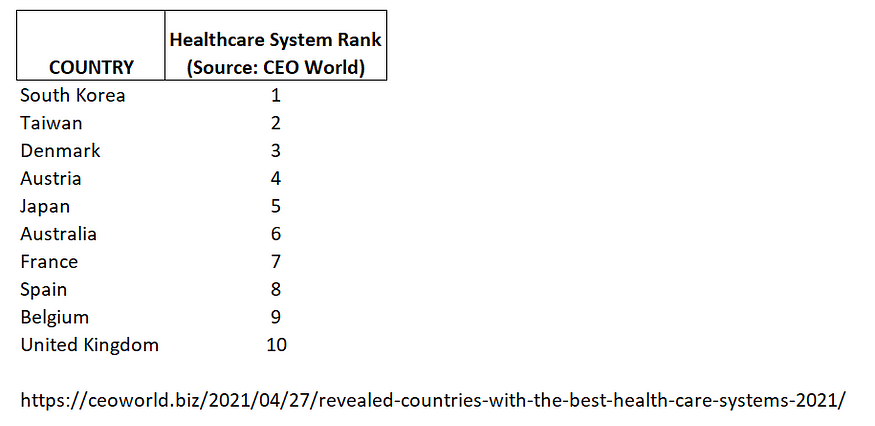
Figure 1b: Bottom10 healthcare systems in the world (Source: CEOWorld Magazine)
Likewise, Figure 2 (below) plots the quality of a nation’s healthcare system by COVID-19 deaths per 1 million people. Ostensibly, there does not appear to be a strong linear relationship between those two variables.
Figure 2: A cross-national comparison of healthcare system quality and COVID-19 deaths per capita.
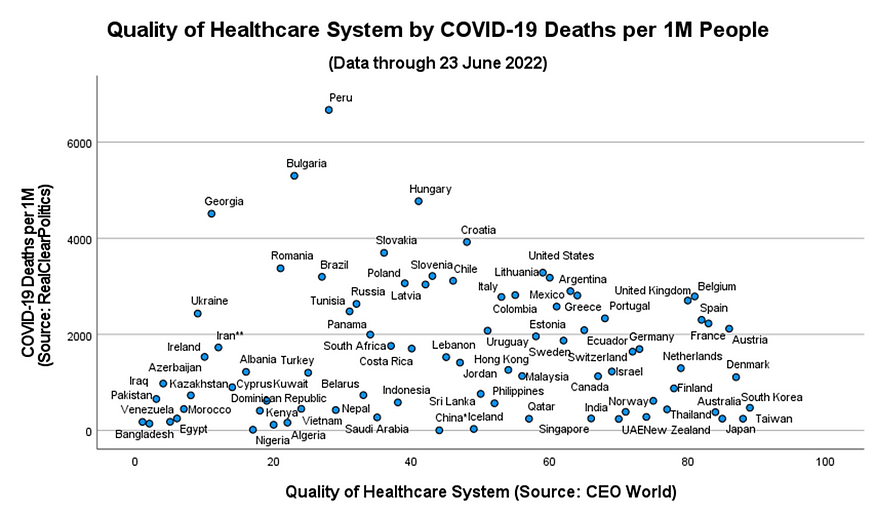
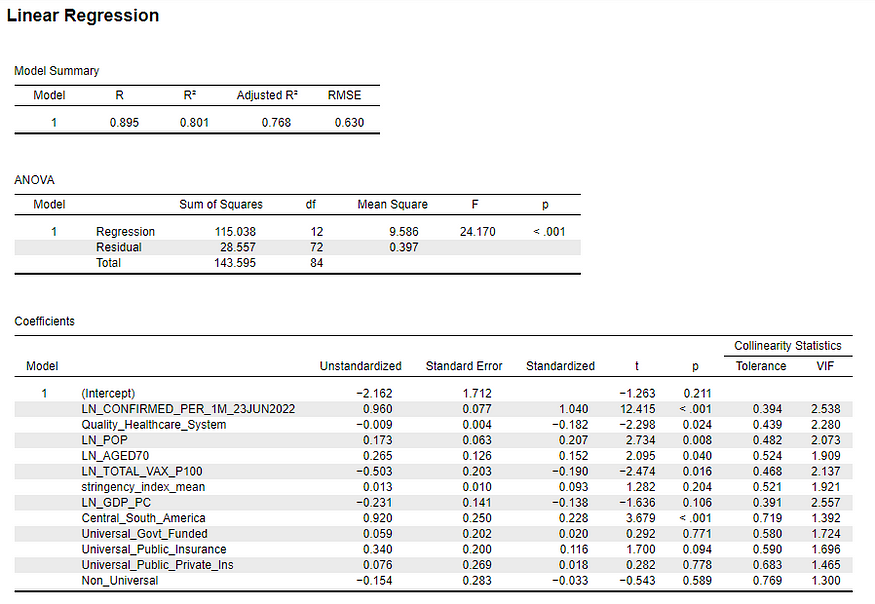
However, in a linear model controlling for COVID-19 incidence (i.e., confirmed cases per capita), population size, age distribution, GDP per capita, vaccination rate, and the stringency of COVID-19 policies, the quality of a nation’s healthcare system proved significant across all of the models tested. The parameter estimates (and diagnostics) for the final, reduced model are shown in Figure 3.
Figure 3: A linear model explaining COVID-19 deaths per capita in 85 countries.

Methodological Note:
One of my subscribers asked how the results in Figure 3 would change if China and Venezuela were removed from the analysis, as many analysts have contended that both countries have not been forthright in their COVID-19 reporting.
Their removal did not change the substantive findings in Figure 3, and though I don’t report the results excluding China and Venezuela here, I can provide them upon request. And, as always, the raw data is available on Github for others to analyze.
Based on their standardized parameter estimates, the number of confirmed cases per capita (β = 1.03),a country’s population size (β = 0.24) and the quality of its healthcare system (β = -0.24) were the best predictors of COVID-19 deaths per capita.
The higher a country’s population, the higher the number of COVID-19 deaths per capita.
The better the quality of country’s healthcare system, the lower the number of COVID-19 deaths per capita.
Other significant predictors of COVID deaths per capita were vaccination rates, the percentage of citizens over 70, and the average stringency of COVID-19 policies (from 1 January 2020 to 23 June 2022).
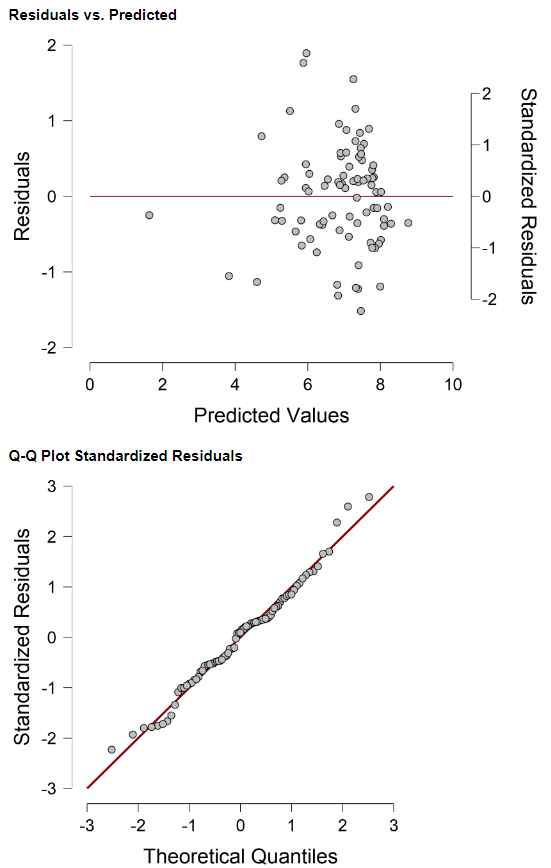
Overall, the reduced linear model in Figure 3 explains 73 percent of the variance in COVID-19 death rates. [The reduced model’s residuals are plotted in Appendix B.]
Some will be perplexed that the regression parameter for policy stringency is positive — which implies that the stricter the COVID-19 policies, the higher the COVID-19 death rate per capita.
In a static, cross-sectional analysis this analytic outcome makes empirical sense. It is not surprising that countries facing the worst COVID-19 outcomes would impose the strictest policy measures. This finding, however, does not in any way suggest that COVID-19 mitigation policies didn’t work. In fact, my own time-series analysis in this area says otherwise: Proactive COVID-19 policies worked better than reactive policies.
In any case, simple assumptions about the effectiveness of mask mandates, vaccine dictates, business shutdowns, school closings and social distance requirements should always be subject to empirical analysis.
But the purpose of this data essay is not to argue the effectiveness of COVID-19 policies — it is to argue whether human lives could have been saved in the U.S. had the country a better healthcare system.
Using the parameters in Figure 3, we can estimate how many U.S. lives would have been saved had the country’s healthcare system been of a higher quality. The results support the conclusions of the Yale study. If the U.S. had a more equitable healthcare system, hundreds of thousands of lives would have been saved.
Figure 4 presents an estimate of the number of U.S. COVID-19 deaths that could have been avoided had the U.S. a healthcare system comparable in quality to other countries.
Figure 4: How many lives would have been saved if the U.S. had a better healthcare system?
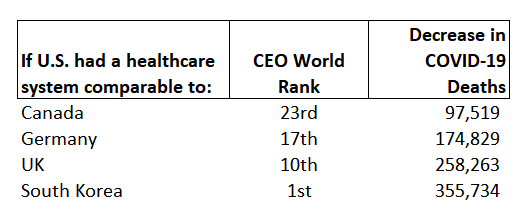
If the U.S. had a healthcare system comparable to our neighbor to the north (Canada), we would have saved almost 100,000 COVID-19 deaths.
A U.S. healthcare system similar to Germany’s hybrid system would have saved a 175 thousand lives. And a U.S. healthcare system at the U.K.’s level of quality would have saved 258 thousand lives.
And if the U.S. had the best healthcare system in the world, as asserted by the Acton Institute, there would be 356 thousand more Americans alive today.
Some last thoughts
The findings from this data essay argue that the U.S. healthcare system is not only inadequate, it has systematically failed at its number one job of taking care of all Americans.
It is not acceptable that American doctors and pharmaceutical executives are millionaires while a million Americans die from a virus that other countries — with superior healthcare systems — were able to contain at a fraction of the human carnage experienced within the U.S.
Dr. Abdul El-Sayed, a physician and progressive candidate in Michigan’s 2018 Democratic gubernatorial primary election, describes the five reasons Medicare-for-All (universal healthcare) is superior to private healthcare:
- Despite political rhetoric suggesting otherwise, there are no free markets in private healthcare
- There is no financial incentive for prevention in private healthcare
- American healthcare is expensive because insurers and hospitals negotiate (collude) with each other
- Sixty-five percent of our healthcare system is already public (Medicare/Medicaid, TRICARE, Veterans)
- Money spent inefficiently on healthcare is money not spent on other important problems (e.g., climate change)
Historical trends in U.S. healthcare expenditures reinforces Dr. El-Sayed’s fifth point. In 2020, health spending accounted for one-fifth (19.7%) of the total U.S. economy (see Figure 5). Fifty years ago, it was a mere 6.9 percent of the economy.
Figure 5: Annual U.S. health expenditures (US $ per capita, 1970–2020)
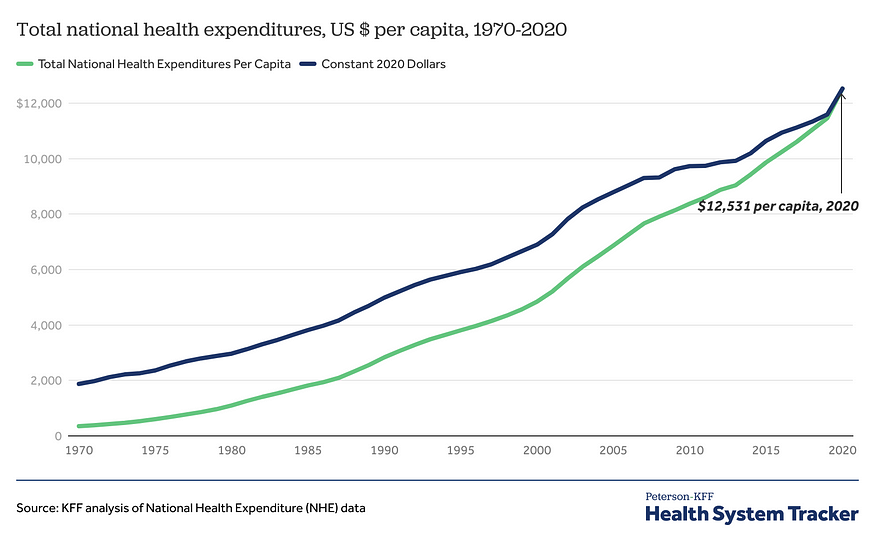
While exacerbated by the COVID-19 pandemic, the upward trend in U.S. healthcare spending established itself long before 2020. In a country where treatment of a snake bite can cost over $140,000 (if helicopter transport is required), the rise in healthcare costs is not an economic abstraction. It is real. And we will never contain these cost increases until we abandon half-measure reforms (think: Obamacare) and, instead, pursue fundamental, structural reform.
And, according to Yale’s Center for Infectious Disease Modeling and Analysis, the most logical and attainable policy choice is universal public healthcare under a Medicare-for-All system.
Will it happen? I doubt, as we have two Right-leaning parties dominating our political system right now.
- K.R.K.
Send comments to kroeger98@yahoo.com
Appendix A: Full linear model with GDP per capita, Central/South America, and healthcare system type controls (Dependent Variable: COVID-19 deaths per capita)
Appendix B: Linear model residuals (Dependent Variable: COVID-19 deaths per capita)