By Kent R. Kroeger (Source: NuQum.com; May 13, 2022)
Disclaimer: I am statistician by training, freelance writer by choice, and an auditor at Amazon out of financial necessity. All grammatical errors and factual inaccuracies in this essay are mine alone. And, as always, do not make financial, medical or personal decisions based on the contents herein.
“Wishful thinking is one thing, and reality another.”
— Jalal Talabani (former President of Iraq)“Where there is life, there is wishful thinking.”
— Gerald J. Lieberman (author)
One controversy I’ve generally avoided writing about is the disputed effectiveness of ivermectin in the treatment of COVID-19, a drug that is an empirically-proven treatment for parasites in humans and animals and whose discoverers won the 2015 Nobel Prize in Medicine for their effort.
But a drug that works for parasites is not necessarily effective in treating (or preventing) COVID-19. That conclusion requires significant direct evidence.
The initial optimism in ivermectin’s use for COVID-19 was rooted in indirect evidence with multiple pre-COVID-19-pandemic studies showing that ivermectin has antiviral properties against a variety of viruses, including influenza, Zika, HIV, and Dengue (a representation of these peer-reviewed studies is found here, here, here and here).
But the interest in ivermectin as a COVID-19 treatment accelerated after an in vitro study by Caly et al. (2020) reported that ivermectin significantly inhibits SARS-CoV-2’s replication in a cell culture model. [SARS-CoV-2 is the virus that causes COVID-19.]
At the onset of the COVID-19 pandemic there was substantial scientific evidence to warrant calls for more systematic research on the potential use of ivermectin in the treatment or prevention of COVID-19, but it was the intersection of this prior research with an understandable desire to find a cost-effective treatment for COVID-19 that ultimately drove mass interest in ivermectin.
No conspiracy theory or fake news fancy drove interest in ivermectin — to the contrary, it was scientists, physicians, and public health experts who wanted to find a cost-effective COVID-19 treatment that could be deployed in parts of the world where prohibitively expensive treatments and vaccines were not an affordable option.
The current list of “Centers for Disease Control and Prevention (CDC)-approved” COVID-19 treatments is currently defined by expensive drug treatments:
Remdesivir costs $2,340 for a five-day course treatment for COVID-19. While Pfizer’s antiviral, Paxlovid, costs $530 for a five-day course, and Merck and Co.’s antiviral, Molnupiravir, costs $700 per five-day course. In addition, Sotrovimab, an intravenous monoclonal antibody drug developed by GlaxoSmithKline and Vir Biotechnology Inc. costs $2,100 per treatment course.
By comparison, the vaccines are significantly more affordable than post-infection treatments, but in a world where two-thirds of all people live on less than $10-a-day, the costs for COVID-19 vaccinations are also exceedingly exorbitant to billions of people.
Among the mRNA vaccines (i.e., Pfizer and Moderna), the Centers for Medicare & Medicaid Services is reimbursing providers about $40 for each shot of the vaccine they administer in order to cover the labor involved.
If you are like me, you are on COVID-19 booster shot number two.
Simply put, even if these vaccines were available to everyone on the planet (they aren’t!), the costs associated with them are not an option for the majority of humans.
Hence, a deep and profound interest in cheap treatment alternatives — call it wishful thinking— has driventhe worldwide interest in drugs such as ivermectin.
In contrast, the mainstream media in the U.S. has aggressively (and cruelly) impugned the motives of anyone suggesting ivermectin is a useful treatment for COVID-19.
Unfortunately, for everyone invested in this debate, the science for and against ivermectin in the treatment of COVID-19 is not clear enough from a statisticians point-of-view to justify either side from claiming the highroad.
I do not know what value ivermectin offers in combating COVID-19.
Instead, wishful thinking seems to be driving most of the narrative on ivermectin. On one side are the ivermectin advocates who are driven by an understandable belief that affordable treatments for COVID-19 already exist and will be crucial in mitigating the impact of this virus, particularly in the developing world. On the other side are economically powerful entities (with well-funded lobbying efforts) who are determined to stamp out resistance to the proprietary, highly-profitable vaccines and treatments currently approved by the U.S. Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC). However, these anti-ivermectin forces cannot wish away the evidence showing that ivermectin may work to some degree against COVID-19.
Personally, I don’t believe the statistical evidence is strong enough to support ivermectin as a substantive treatment for COVID-19. From the reported clinical results I’ve seen, ivermectin offers, at best, only a marginal improvement in COVID-19 outcomes.
But that is not the same as saying ivermectin has no medical value in combating COVID-19. That conclusion is not obvious.
Even good science contains flaws
To shame those interested in ivermectin, the news media’s chosen posterchild for allegedly biased and fraudulent ivermectin research is an 2020 Egyptian clinical study led by Dr. Ahmed Elgazzar, a medical researcher at Benha University (Egypt). The randomized-controlled-trial (RCT) study he led of ivermectin’s effectiveness against COVID-19 was rightfully questioned for its poorly-documented random assignment protocols in which the control group (i.e., did not receive ivermectin treatment) was entirely drawn from intensive care units (ICU), but where the treatment group (i.e., received ivermectin) was drawn from both ICU and normal hospital care instances.
The critical component of an RCT study is that assignment to the control and treatment groups is entirely random. It is not clear that Elgazzar’s Egyptian study followed that requirement.
Though Elgazzar contends his study was withdrawn from publication before he was given a sufficient opportunity to address the study’s problems, the consequence is that his study contaminated the credibility of other ivermectin study’s that found some treatment effectiveness against COVID-19.
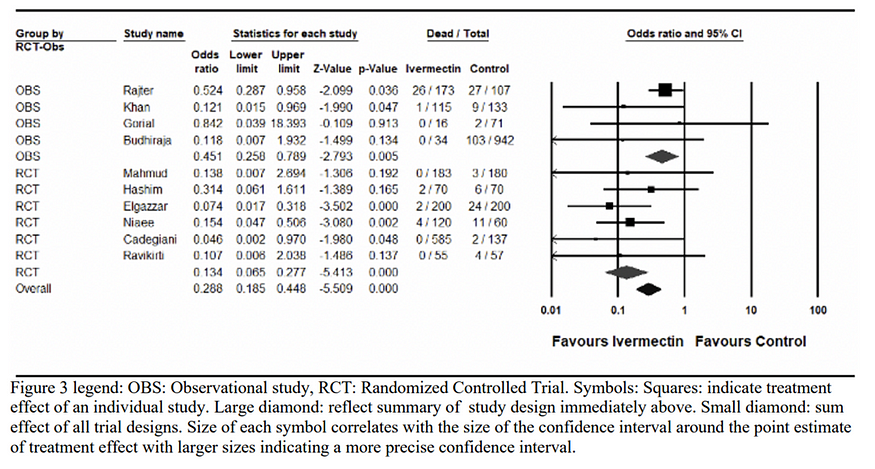
So when a meta-analysis of ivermectin’s effectiveness by Kory, Pierre, MD, et al. (“Review of the Emerging Evidence Demonstrating the Efficacy of Ivermectin in the Prophylaxis and Treatment of COVID-19.” 13 Nov. 2020) originally included the Elgazzar et al. study in its analysis (see Figure 1 below), the news media understandably questioned their conclusions.
Figure 1: Meta-analysis of the outcome of mortality from controlled trials of ivermectin treatment in COVID-19 [reprinted Figure 3 in original Kory, et al.(2021)]; (Odd-ratios estimates below 1.0 with credible intervals not containing 1.0 indicate ivermectin’s effectiveness against COVID-19)
The original publisher of the Kory et al. study sensibly issued a disclaimer:
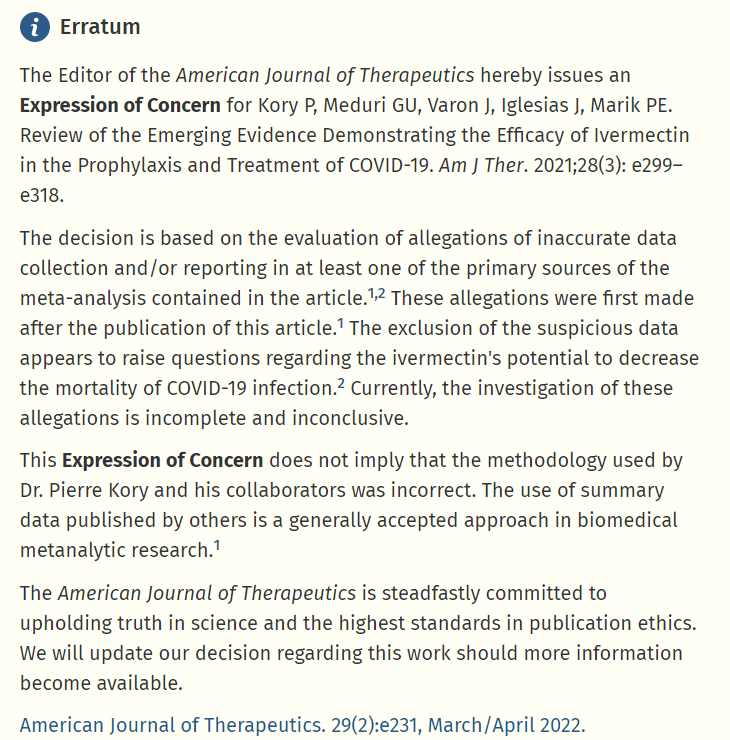
That is exactly what good science should be doing — questioning the findings of researchers using flawed or questionable methods.
If only the large pharmaceutical companies faced similar challenges.
Dr. Kory and his coauthors issued a response to the editors of the American Journal of Therapeutics:
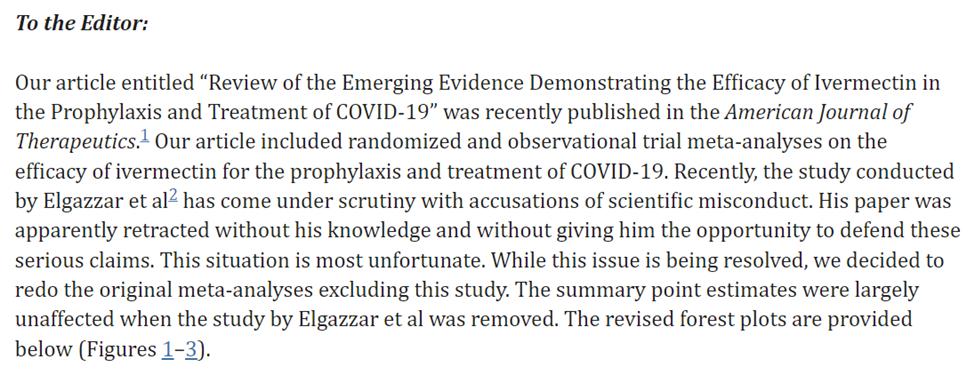
Their revised meta-analytic summary of ivermectin’s effectiveness was mostly unaffected by the exclusion of the Elgazzar et al. study (odd-ratios below 1 indicate ivermectin’s effectiveness against COVID-19):
Figure 2: Revised Figure 3 table in Kory, et al.(2021)
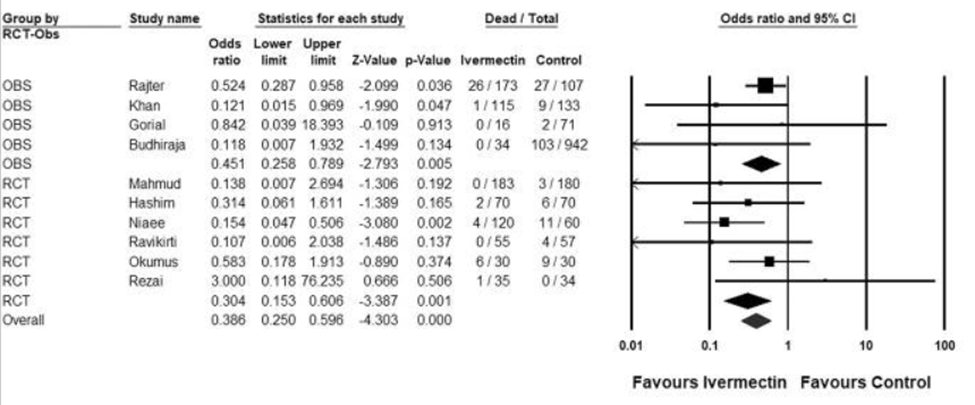
Because of the obvious flaws in the Elgazzar et al. study, are we to assume all research supporting ivermectin as an effective treatment for COVID-19 are equally suspect?
It is an archetypalexample of white European arrogance to suggest good science is not conducted in countries like Bangladesh, Brazil, India, Iraq, and Iran.
There are well-trained medical research methodologists in all of those countries.
The developed world’s impulsive rejection of ivermectin as a treatment for COVID-19 is unfortunate. The objective facts suggest ivermectin has some value against COVID-19.
Which brings us to the media-trumpeted study that purportedly proved that ivermectin does not positively impact COVID-19 outcomes.
The news media openly promotes bad research
The Together Study conducted in 2021 by Brazilian medical researchers concluded that ivermectin had no substantive impact on COVID-19 outcomes.
The American news media couldn’t be happier, as evidenced by these emphatic headlines:
Ivermectin Does Not Reduce Risk of Covid Hospitalization, Large Study Finds — The New York Times, March 30, 2022
Ivermectin does not prevent COVID-19 hospitalization, a new study says — NPR News, March 30, 2022
Study finds ivermectin, the horse drug Joe Rogan championed as a COVID treatment, does nothing to cure the virus — Fortune.com, March 31, 2022
Unfortunately, the research the mainstream media used to dismiss ivermectin was hardly better than the research supporting its effectiveness.
Like the Elgazzar et al. study, the Together Study had a curiously suspicious treatment/control group problem. A significant percentage of the control group in the Together Study (i.e., did not receive ivermectin) did not complete the study (see Figure 3). Where originally 679 COVID patients were assigned to the control group, only 228 were included in the ‘per-protocol’ analysis (i.e., followed the proper control procedures).
Figure 3: Sample disposition from the 2021 Together Study
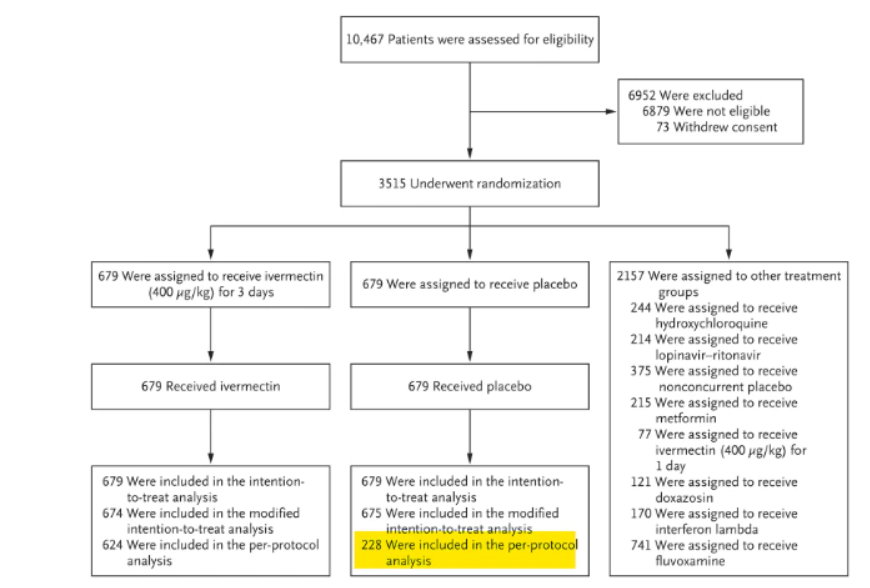
More in-depth statistical critiques by Phil Harper and Alexandros Marinos of the Together Study can be found here and here, but the strange dropout of 451 control group participants during the course of the study begs one fundamental question: What happened during this study that would cause 451 people in the control group to violate protocols?
A plausible explanation is that these control group participants “learned” that they were not receiving the ivermectin treatment and decided to drop out of the study in order to receive that treatment. But that is pure speculation.
Harper states the potential ramifications of the control group dropout problem:
The ivermectin arm should have reported 21 deaths in 624 patients, as that’s how many patients fully completed the study. The placebo group should have reported 24 deaths in 288 patients, as that’s how many patients fully completed the study.
Instead each arm reported the number of deaths among the number of patients initially enrolled even though those patients did not complete the study. By not comparing like for like groups, all notions of ‘randomized control’ are gone from the trial, and it drastically alters the results.
These issues warrant an official response from the New England Journal of Medicine.
Putting aside the Together Study’s per-protocol sample problems, I am nonetheless drawn to the study’s statistical analyses that found a roughly 80 percent probability that ivermectin’s treatment value exceeded that of the placebo (see Figure 4). It is not significant by strict statistical standards, but it is suggestive that a more rigorous study might reveal a genuine benefit from ivermectin’s inclusion in a COVID-19 treatment program.
Figure 4: Probability of efficacy and Bayesian relative risk of COVID-19 hospitalization or extended emergency room observation for ivermectin vs. placebo taken from the 2021 Together Study
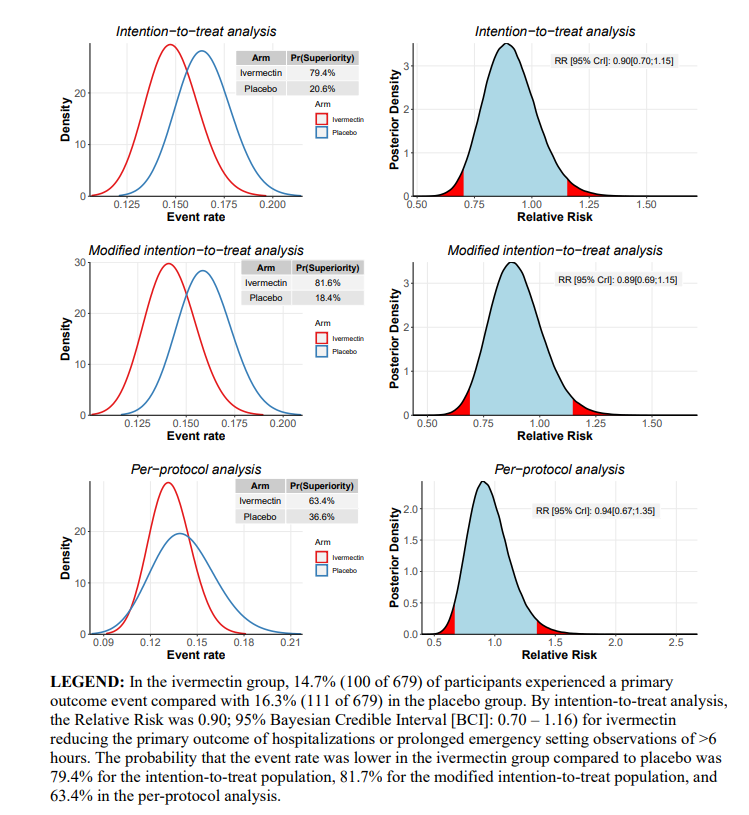
If anything, the Together Study increases my belief that ivermectin might be an effective treatment option for COVID-19 patients. But, of course, that is in direct opposition to the conclusions drawn in the news media.
We may never know the motives of control group participants who left the Together Study without significant follow-up research, but the more important point is that flawed research posed against other flawed research is not a formula for understanding the value of ivermectin against COVID-19.
Partisan and corporate interests are destroying the credibility of scientific inquiry.
That is not a good omen for our ability to incorporate quality science into the public policymaking process going forward.
Final Thoughts
As noted, there was enough circumstantial evidence at the beginning of the COVID-19 pandemic to justify calls for RCT research on ivermectin’s potential repurposing for use against COVID-19.
Did it happen? Yes, but not in the U.S. or Europe. Rather, the early ivermectin RCT research occurred in countries where there was already substantial human-treatment experience with the drug for parasites (Bangladesh, Brazil, India, Iraq, and Iran).
Among the first RCT U.S. studies of ivermectin and COVID-19 is ACTIV-6, a nationwide, double-blind clinical study led by Duke University’s Clinical Research Institute, which announced in August 2021(!) that the study would start including ivermectin as one of the repurposed drugs to be tested (along with Fluticasone and Fluvoxamine).
August 2021? Really? If ivermectin warranted study in August 2021, why not in August 2020? Or April 2020? Why the delay? My hunch…my fear…is that the combination of powerful private interests (i.e., the pharmaceutical industry, which funds most clinical trials in the U.S.) and toxic political partisanship killed any chance ivermectin ever had to be included in the early COVID-19 treatment research.
Even ivermectin is not an effective treatment for COVID-19, the fact that it took a year-and-a-half before the U.S. medical research community took any meaningful effort to study its treatment value is scientific malfeasance. If it turns out that ivermectin is an effective treatment option, it becomes criminal negligence.
- K.R.K.
Send comments to kroeger98@yahoo.com
