By Kent R. Kroeger (Source: NuQum.com, March 26, 2020)
Nobody truly knows when the coronavirus pandemic will end and its final human toll.
That doesn’t stop some of us from trying to predict how this crisis will resolve.
I predicted in late January that the coronavirus (2019-nCoV) — the virus that causes the COVID-19 disease — would peak in China in mid February around 20,000 cases, effectively joining the pantheon of pandemic scares that never materialized in a big way on a global scale (e.g., 1976 Swine Flu, 2002 SARS, 2012-present MERS, etc.).
After that bad call, I’m officially out of the coronavirus prediction business.
I know I don’t know what is ultimately going to happen with COVID-19.
But the real experts don’t know either.
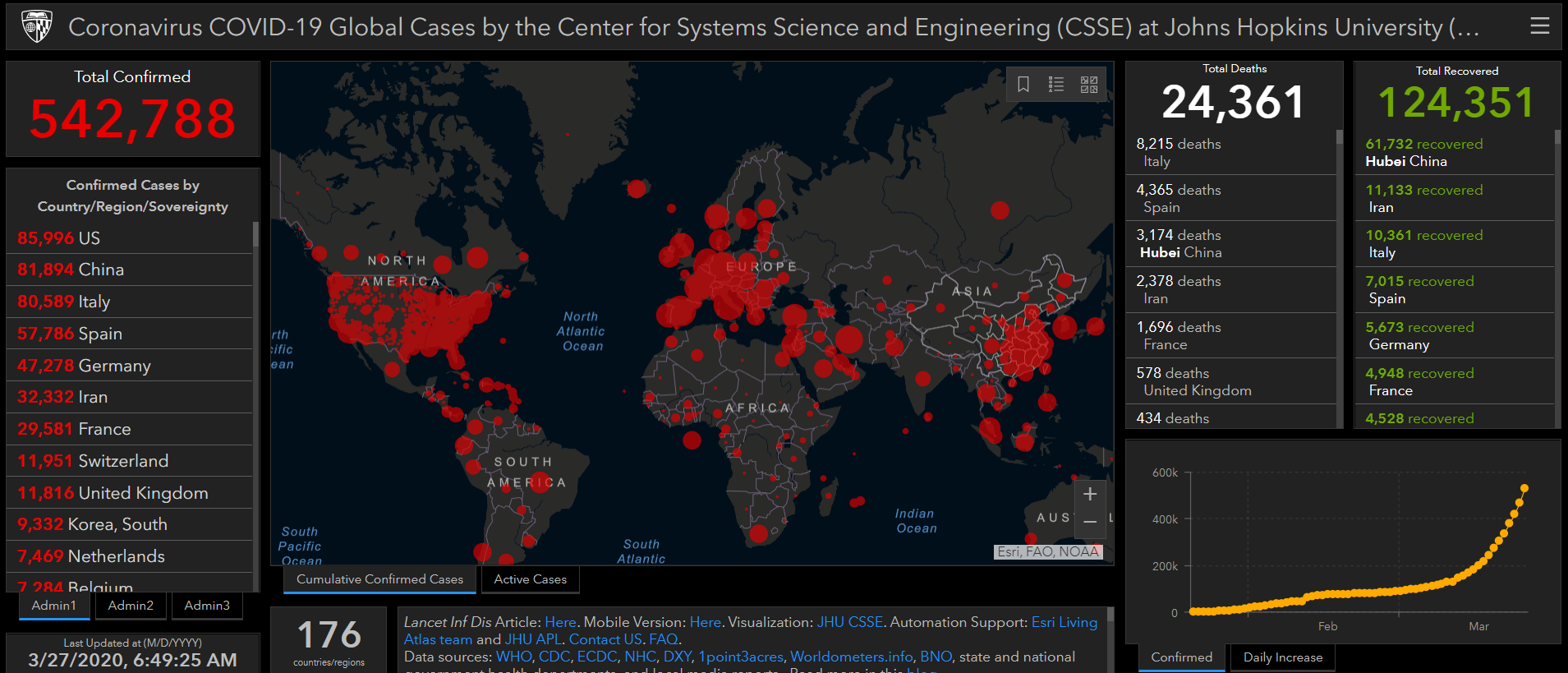
Most of us have visited the Johns Hopkins University (CSSE) website that provides “near real-time” counts of coronavirus COVID-19 cases and deaths worldwide.
Their website has numbers — lots of them — from reliable government sources, nonetheless. Those numbers must be fairly accurate, to the extent possible under such difficult circumstances, right?
Well, no. We don’t know the accuracy of the WHO/JHU(CSSE) numbers are yet.
Scientists who think most about viruses and pandemics are only now beginning the process of understanding the true numbers surrounding this pandemic and how it will end — and we know it will end, someday.
When viewed across countries, the numbers reported by the World Health Organization (WHO) and the JHU (CSSE) website should be taken with a grain of salt. These numbers are probably significant under-counts of the true numbers of COVID-19 cases and related-deaths — numbers that we will know with some confidence perhaps many months (or even years) from now.
At some point, probability samples within those countries most affected by the coronavirus will reveal the percentage of their populations with the virus’ antibodies, indicating how many people were actually infected.
Those types of epidemiological studies take time and aren’t amendable to the 24-hour news cycle that drives our current dialogue around the coronavirus.
Yet, we need good information about the coronavirus now, not eight months from now. Effective public policy requires as accurate, timely information. How contagious is the coronavirus? What is its mortality rate? How does its mortality rate vary by demographic categories (i.e., who is most vulnerable)? What percentage of those infected with the virus failed to ever show symptoms?
________________________________________________________________
The problem is that there is no single simulation model for assessing the trajectory of a pathogen like the coronavirus. Different models, requiring a different sets of assumptions, can render different conclusions. May the best model win.
Presently, a disagreement between two academic groups in the United Kingdom studying the coronavirus highlights this analytic mélange.
In one corner are researchers from Imperial College (London, UK) who, after exhaustive research on individual-level coronavirus transmission dynamics, ran simulations on how the coronavirus would put pressure on the Great Britain (GB) and US health care systems depending on the non-pharmaceutical interventions (NPIs) adopted by the two countries.
Should either country fail to adopt any control measures, according to the Imperial College study, GB and the US can “expect a peak in mortality (daily deaths) to occur after approximately 3 month.”
“In such scenarios, given an estimated R0 of 2.4, we predict 81 percent of the GB and US populations would be infected over the course of the epidemic,” the study concludes. “For an uncontrolled epidemic, we predict critical care bed capacity would be exceeded as early as the second week in April, with an eventual peak in ICU or critical care bed demand that is over 30 times greater than the maximum supply in both countries.”
[R0 represents the expected number of infection cases directly generated by one infected person in a population where all individuals are susceptible to infection.]
That’s the worst-case scenario.
In contrast, the study finds that the most effective combination of interventions is predicted to be “a combination of case isolation, home quarantine and social distancing of those most at risk (the over 70s).”
The Imperial College study is credited with changing GB policy on the coronavirus almost immediately upon its release.
In another corner, researchers from Oxford University (UK), employing a different simulation method, come to a drastically different conclusion about the coronavirus.
“The results we present (in this study) suggest the ongoing epidemics in the UK and Italy started at least a month before the first reported death and have already led to the accumulation of significant levels of herd immunity in both countries,” write the authors of this, as yet, unpublished study.
Herd immunity is critical in dampening or stopping the spread of a virus like the coronavirus. The higher the population percentage already carrying the virus antibodies, the less likely the virus can spread within those still vulnerable to it.
The Oxford study suggests that the overwhelming majority of those infected by the coronavirus never become sick enough to need hospital care. The public policy implications are profound: The coronavirus was spreading rapidly within the population at least a month before the first case was confirmed. In other words, it may be too late for any suppression and mitigation strategies to have a major impact on the trajectory of the coronavirus. The cake is already baked, as they say.
Despite the study’s key findings, the study’s lead researcher Professor Sunetra Gupta, still believes behavioral changes, such as social distancing and self-quarantines, will still be effective at reducing the number of people who become seriously ill due to the virus.
Even if the Oxford study is found to be substantively wrong, Professor Gupta understands the magnitude of the research task needed to render that conclusion: “We need immediately to begin large-scale serological surveys — antibody testing — to assess what stage of the epidemic we are in now.”
[I should note that the Oxford study has come under intense criticism from some prominent epidemiologists since it was released to the media. A sense of that criticism can be found here.]
________________________________________________________________
It is popular in some circles now to dismiss the coronavirus pandemic as more media hype than a globe-threatening health crisis. And, superficially, the numbers support that cynicism.
As of 8:15am today (March 27, 2020), the coronavirus has killed a reported 24,361 people worldwide. There have been five other pandemics in the past 125 years with death tolls far greater than the 2019 coronavirus.
Figure 1: Previous pandemics (Name, Time Period, Source, Death Toll)

HIV/AIDS has killed over 25 million people since its first case in 1981. That is about 625,000 people a year. The 2009–10 Swine Flu killed 200,000 people worldwide (12,000 in the U.S.). The first pandemic I vaguely recall — the 1968–70 Hong Kong Flu — killed 1 million people worldwide, including 100,000 in the U.S.
I don’t recall large chunks of the U.S. going into a stay-at-home lockdown in 2009 (…because we didn’t). There weren’t daily presidential news conferences about the Hong Kong Flu in 1969.
Why is the coronavirus being treated differently?
Keeping in mind that the statistics for the new coronavirus (COVID19/2019-nCoV) are moving targets (for example, estimates on its mortality rate range from 1 to 3 percent), the panic over this latest pandemic most likely stems from the combination of its contagiousness and mortality rate.
The 2014–16 (West African) Ebolavirus killed almost half of the 29,000 people that contracted the virus. It had a high mortality rate, but was geographically concentrated. While it was highly contagious, its symptoms were quite visible and the ability to identify and isolate its carriers much easier than the coronavirus.
The two other coronavirus outbreaks (SARS, MERS) were qualitatively different from the current coronavirus outbreak as well. While SARS had a mortality rate around 10 percent, it was less contagious than 2019-nCoV and, in the end, only infected 8,500 people (mostly in China).
The ongoing MERS outbreak has killed 912 people out of the 2,494 who have contracted the virus (a more than 30% mortality rate). But, again, MERS has been geographically isolated and does not appear to be nearly as contagious as 2019-nCoV.
The 2009 Swine Flu is perhaps the most instructive comparison to 2019-nCoV. Like the current coronavirus, the 2009 pandemic received considerable media attention when the WHO announced the potential for a global pandemic from this new H1N1 flu virus in April 2009. However, in the end, the 2009 Swine Flu’s mortality rate of roughly 0.1 percent was not substantially different from the common flu; and, while 12,000 people did die in the U.S., perceptually it felt like just a “bad” flu season.
The new coronavirus (2019-nCoV) is fundamentally different from these other pandemics. Where the common flu typically has a mortality rate around 0.1 percent (1 in every 1,000 cases), the current coronavirus most likely has a mortality rate at least 10 times more lethal.
Lastly, the numbers commonly cited for pandemics such as the 2009 Swine Flu are epidemiological estimates derived after those outbreaks have ended. Epidemiologists go back into the aggregate diagnostic and mortality data and look for evidence of what impact the pandemic virus may have actually had (beyond simply what was reported contemporaneously). They make sophisticated estimates with known (and unknown) amounts of error. \
The numbers for COVID-19 are reported to the WHO by national health ministries. At a minimum, we know by anecdote that not everyone who contracts a virus goes to the hospital. Many (maybe most) resort to home-care and never seek medical attention. Some will contract a virus and never exhibit symptoms. Evidence of this latter fact comes from the NBA where hundreds of players and coaches exposed to carriers of the coronavirus were tested.
“Following two players testing positive last week, others were tested and five additional players tested positive,” the NBA issued in a statement last week. Since March 11, when Utah Jazz player Rudy Gobert was the first NBA to be diagnosed with the coronavirus, thirteen other NBA players have tested positive. From the most recent information made available to the public, not one of these players has experienced significant symptoms from the coronavirus — which reinforces what may be the most significant feature of the new coronavirus: most infected by it will have no (or only minor) symptoms related to it.
The occurrence of asymptomatic coronavirus carriers has also been revealed by the Germans who have done significantly more coronavirus testing (per capita) than the U.S.
As of March 19, the U.S. had conducted in total only 104,000 tests, according to The COVID Tracking Project. In contrast, according to German health officials, they are equipped to conduct 160,000 tests per week and, unlike the U.S., systematically test people who are not symptomatic. Germany’s broader testing effort is designed to understand the true extent of the coronavirus infection rate and has revealed thousands of Germans who carry the virus but are not symptomatic.
As of March 27, the Germans have reported 304 deaths against 49,344 confirmed cases, for a mortality rate of 0.6 percent — among the lowest rates in those countries most affected by the coronavirus. Some epidemiologists are citing Germany’s effort to identify asymptomatic carriers early as one of the reasons for Germany’s low mortality rate. Identify those infected before they are sick and you increase their chance of a full recovery.
But more than asymptomatic carriers and those who treat their symptoms exclusively at home can fail to get counted by health officials. Research has shown that medical databases are not always accurate. For example, people can die from complications associated with a virus (organ failure, hemorrhaging, etc.) and yet never get classified as having died from the virus if they had not been tested for it.
The reality is that data collection on a scale as large as the coronavirus requires is going to have significant amounts of error through selection bias, incomplete population coverage, coding mistakes and simple random chance.
I will make this one prediction about COVID19: The numbers were are seeing now (as reported to the WHO) are nowhere near the true impact of COVID-19 — particularly in countries with less-developed health care systems and limited resources for health testing and monitoring.
When this is all over, it will take many months before we know what COVID-19 really did.
__________________________________________________________________
Even so, I believe there is evidence in the current COVID-19 data from the WHO that this pandemic will peak soon.
We have already seen countries get control of their first wave of the coronavirus — China, South Korea — and Italy, U.S. and France may be making this critical turn soon (see Figure 2).
Figure 1: Coronavirus trajectories of daily new cases for selected countries
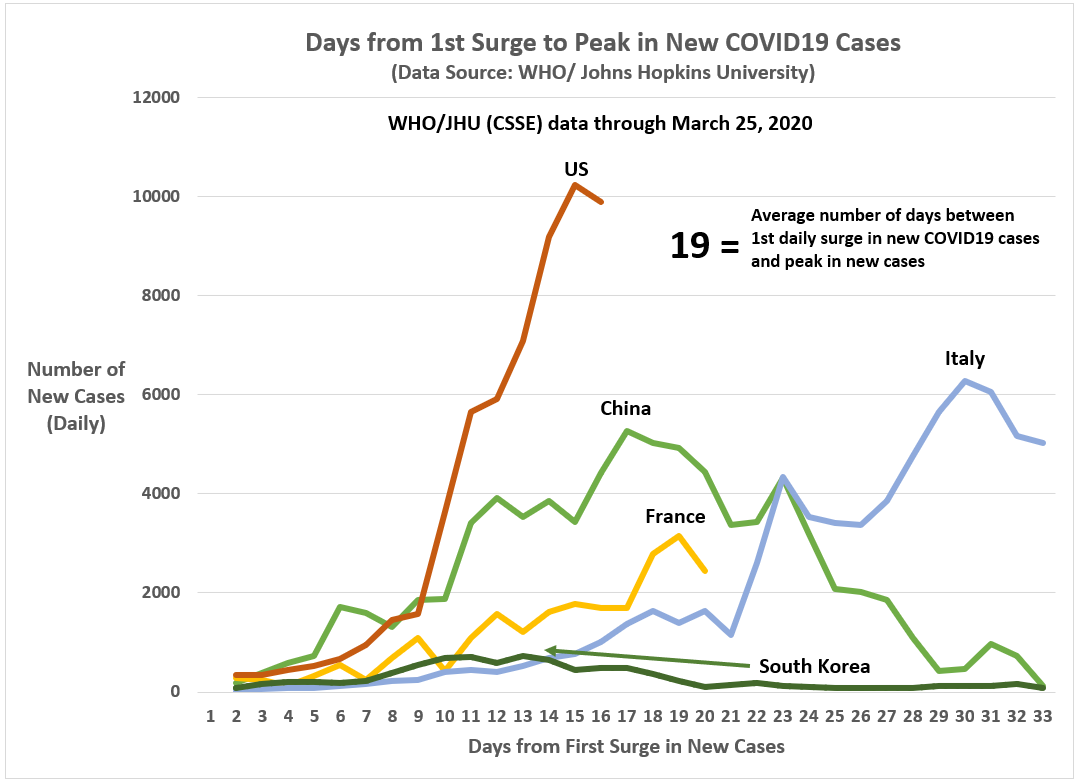
The current coronavirus pandemic will end. It is not a question of if, but one of when.
But I’m not making any predictions.
- K.R.K.
Datasets used in this article are available by request to: kroeger98@yahoo.com