By Kent R. Kroeger (Source: NuQum.com; February 19, 2021)
The U.S. may have experienced 7.7 million additional COVID-19 cases and 155 thousand additional COVID-19 deaths due to its subpar health care system.
This finding is based on a cross-national statistical analysis of 20 West European and West European-heritage countries using aggregate, country-level data provided by Johns Hopkins University (COVID-19 cases and deaths per 1 million people), OurWorldInData.org (Policy Stringency Index) and HealthSystemFacts.org (Health Access and Quality Index). The analysis covers the period from January 1, 2020 to February 5, 2021.
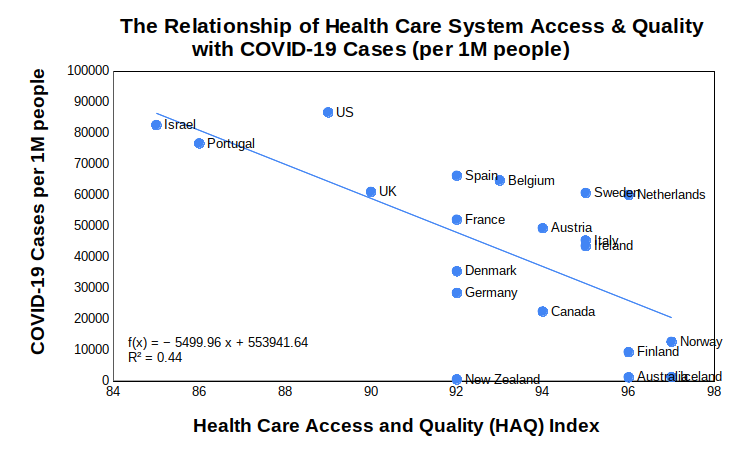
Figure 1 (below) shows the bivariate relationship between the number of COVID-19 cases (per 1 million people) and the quality of a country’s health care system as measured by the Health care Access and Quality Index (HAQ Index ) that was compiled during the 2016 Global Burden of Disease Study.
In countries where health care access is universal and of high quality, the performance on the number of COVID-19 cases per capita is much better. New Zealand, Australia, Iceland, Finland and Norway are positive exemplars in this regard. Israel, Portugal, U.S., and the U.K., in comparison, are not.
Figure 1: Health care access/quality (HAQ) and its relationship to COVID-19 cases per 1 million people
More interestingly, if over the study period we control for the average level of COVID-19 policy actions (as measured by Oxford University’s COVID-19 Government Response Tracker (OxCGRT)) and whether or not a country is an island, the significance of the quality of a country’s health care system remains significant.
As seen in this simple linear regression model, three variables — the HAQ Index, COVID-19 Policy Stringency, and whether or not the country is an island — account for about 60 percent of the variance in COVID-19 cases per capita for these 20 countries.

Using this model, we can estimate the number of COVID-19 cases (per 1 million people) the U.S. would have experienced if its health care system was as good as the countries rated as having the best health care systems in the world (Iceland and Norway — HAQ Index = 97).
(-2946.23 * 8)*330 = 7,778,000 additional COVID-19 cases
[Note: U.S. has approximately 330 million people and its HAQ Index = 89]
Additionally, as there is a strong relationship between the number of COVID-19 cases per capita and the number of COVID-19 deaths per capita (i.e., roughly 0.2 deaths per case — see Appendix), we can estimate that the U.S. has experienced 155,560 additional deaths as a result of inadequacies with its health care system.
The U.S. does not have the best health care system in the world
Remarkably little discussion within the national news media has been about the systemic problems within the U.S. health care system and how those problems contributed to the tragic COVID-19 numbers witnessed by this country during the pandemic. Where most of the media attention has been focused on political failures associated with the COVID-19 pandemic — and most of that has been directed at the Trump administration — the hard evidence continues to suggest systemic factors, such as racial disparities in socioeconomics and health, are driving U.S. COVID-19 case and death rates above other developed countries.
“Socioeconomically and racially segregated neighborhoods are more vulnerable and are more likely to be disproportionately impacted by the adverse effects of COVID-19,” conclude health analysts Ahmad Khanijahani and Larisa Tomassoni. As for why this is the case, Khanijahani and Tomassoni offer this explanation:
“Black and low-SES individuals in the US are more likely to be employed as essential workers in occupations such as food distribution, truckers, and janitors. Most of these jobs cannot be fulfilled remotely and usually do not offer adequate sick leaves. Additionally, individuals of low-SES and Black minority are disproportionately impacted by homelessness or reside in housing units with limited space that makes the practice of isolating infected family members challenging or impossible. Moreover, limited or no child/elderly care and higher uninsurance rates impose an additional financial burden on low-SES families (emphasis mine) making it challenging to stop working.”
The racial and ethnic disparities in COVID-19 death figures (in Figure 2) are shockingly apparent in the following graphic produced by the The Centers for Disease Control and Prevention (CDC).
Figure 2: Racial/ethnic disparities in COVID-19 deaths in the U.S. (Source: CDC)
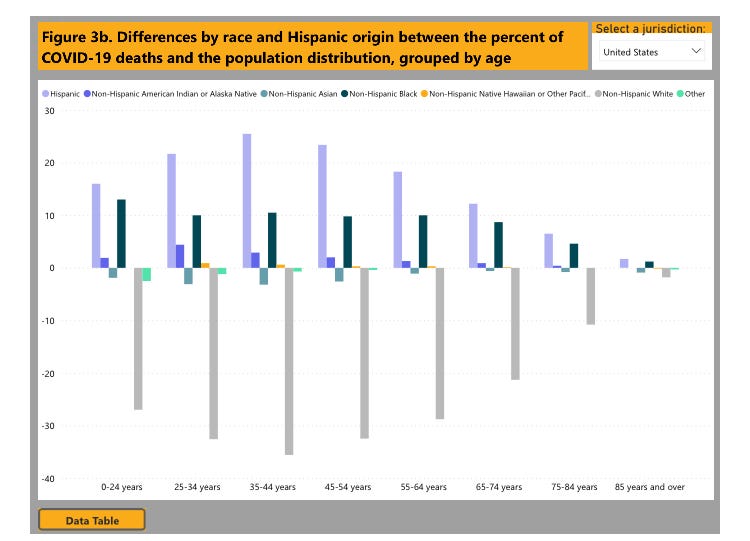
The gray bars in Figure 2 show how non-Hispanic Whites across all age categories have experienced fewer deaths than expected relative to their prevalence in the total U.S. population. In stark contrast, across all age groups, Hispanic and non-Hispanic Blacks account for a significantly higher percentage of COVID-19 deaths than expected based on their population numbers.
Figure 2 is what a broken health care system interacting with systemic racial and ethnic inequalities looks like in a chart.
Final thoughts
Citing the negative role of the U.S. health care system on COVID-19 outcomes is not an indictment of U.S. health care workers. To the contrary, because Americans live in a country where health care is significantly rationed by market forces — e.g., a relatively high rate of uninsured, people delaying preventative care, diagnoses and treatments due to financial concerns, etc. — our health care workers are forced to work harder as a high number of COVID-19 patients enter the health care system only after their symptoms have already become severe.
The awful impact of the COVID-19 pandemic on Americans is less a political failure than it is a systemic failure —though we cannot dismiss the ineptitude of politicians like New York Governor Andrew Cuomo who, presumably at the behest of his health policy experts, authorized sending critically ill seniors from hospitals to nursing homes in order to free up hospital beds. New York’s elderly paid a steep price so Governor Cuomo could learn that nursing homes are not hospitals.
More broadly, the COVID-19 pandemic exposed a broken and inadequate U.S. health care system that is better designed to protect high profit margins for insurance and pharmaceutical companies and the billing rates of physicians than it is to ensure the health of the American people.
Sadly, with the physician, health insurance and pharmaceutical lobbyists firmly entrenched in the policymaking machinery of the Biden administration, don’t expect any time soon the types of health care system reforms needed to fix our systemic problems.
- K.R.K.
Send comments to: nuqum@protonmail.com
Methodological Note:
The decision to analyze just 20 West European and West European-heritage countries (i.e., U.S., Israel, Canada, Australia, and New Zealand) was prompted by a desire to control for two factors that are significantly related to country-level COVID-19 outcomes: (1) cultural norms, and (2) economic development.
Controlling for cultural norms, particularly the differences between countries with individualistic cultures (i.e., Western European nations) and those with collectivist cultures (i.e., East Asian nations), facilitated a clearer look at the impact health care systems on COVID-19 outcomes.
As for the exclusion of lesser-developed countries from this analysis, I simply don’t trust the accuracy or completeness of their COVID-19 data.
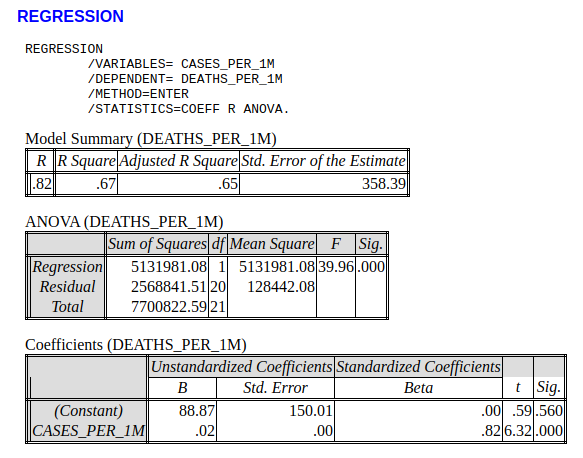
APPENDIX — A Linear Model of COVID-19 Deaths (Per 1 Million People)